-
News & Events

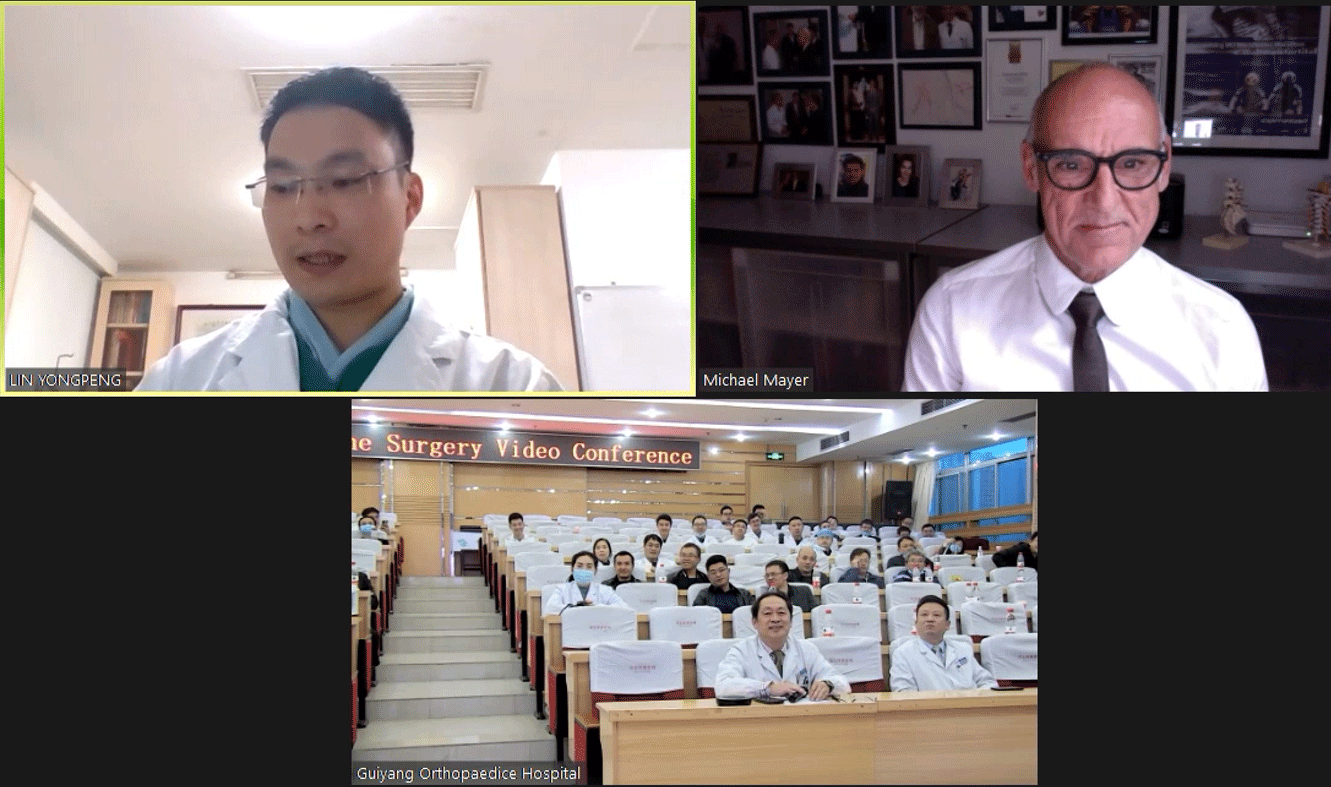
Sino-German Spine Surgery Video Conference was held in the afternoon of November 6th at The Fourth People’s Hospital of Guiyang. The video conference was successfully organized by The Fourth People’s Hospital of Guiyang and co-organized by The Third Affiliated Hospital of Army Medical University, The Second Affiliated Hospital of Kunming Medical University, Affiliated Hospital of Chengdu University of Traditional Chinese Medicine. And We are so honored to invite Prof. Mayer, the Founding President of German Spine Society and Former President of European Spine Society to join us. Xiao Jie, Director of Spine Surgery of The Fourth People’s Hospital of Guiyang served as the host at this conference and Lin Yongpeng, Doctor of OrthopedicsⅠ(Spine Surgery) of Guangdong Provincial Hospital of Chinese Medicine acted as the interpreter. Additionally, three case discussion reports were presented respectively by Doctor Tian Zhen,Doctor Feng Mingxing and Doctor Zhang Yang of The Fourth People’s Hospital of Guiyang.


Long Shengli, Vice President of The Fourth People’s Hospital of Guiyang, on behalf of the hospital, expressed his warmest welcome to Prof. Mayer, specialists and colleagues and thanks to all fellow hospitals for their concerns and support to construction and development of our hospital as always. He also expressed that it was a great honor to have Prof. Mayer, the world-known master on minimally invasive spine, to share his insightful ideas with Chinese colleagues today.
Prof. Mayer gave a lecture of "Degenerative Lumbar Scoliosis - Surgical Aspects, Complications and Other Specifics" . In his lecture, he shared his experience on performing surgeries , avioding compications and so on.
Prof. Mayer said that whenwe deal with degenerative scoliosis in elderly patients, therapeutic goals in treatment should close to relieving pain (in back and leg), preserving mobility and stability instead of correction itself.
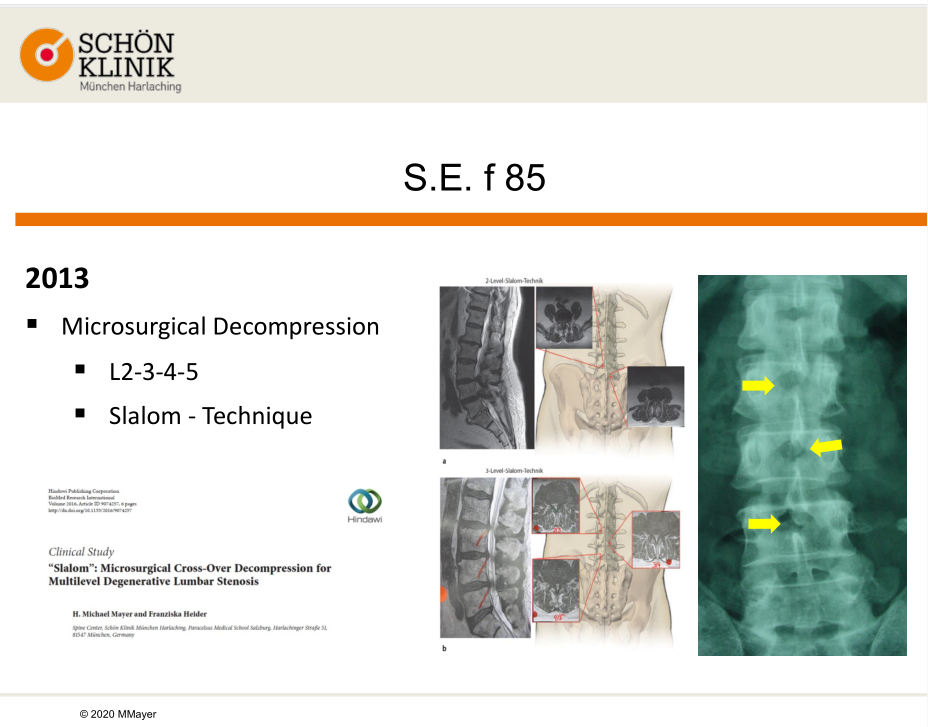
Prof. Mayer shared with us a typical case he encountered in 2013. The patient was an 85-year-old female with a diagnosis of degenerative lumbar scoliosis on L3-4, L4-5 and especially on L2-3. The following treatment was to perform a microscopic decompression of the lumbar on L2-3-4-5 by using a surgical technique called Slalom. Two years later, the patient came back with progressive back pain and groin pain on the right side. At that time she was under conservative treatment with multiple injections, like facets injection and lumbar epidural steroid injections, but with no sustained effect.
Then the proper surgical treatment for an 87-year-old patient was a very important decision, especially when the patient suffered from diabetes mellitus, arterial hypertension, compensated cardial insufficiency and COPD at the same time. Was it right to continue conservative treatment or to do a MIS discectomy on L3-4? If the latter was approved, should it go with or without stabilisation? If it went for stabilisation, which methods should be used? All the factors that mentioned above mattered a lot in coming out a proper solution for the patient. Additionally, it was also very necessary to consider whether the lumbar scoliosis would be progressively degenerative in the future.
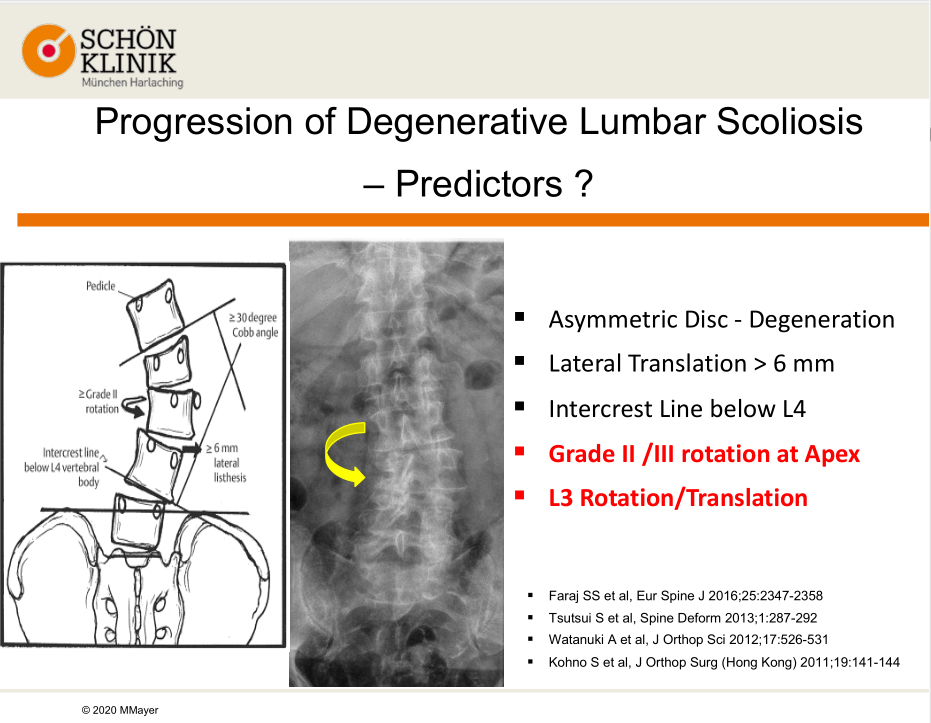
Prof. Mayer also shared his experiences in how to predict if a patient has a progression of degenerative lumbar scoliosis. Here are five predictors that may help:
1. Asymmetric Disc - Degeneration
2. Lateral Translation > 6 mm
3. Intercrest Line below L4
4. Grade II /III rotation at Apex
5. L3 Rotation/Translation
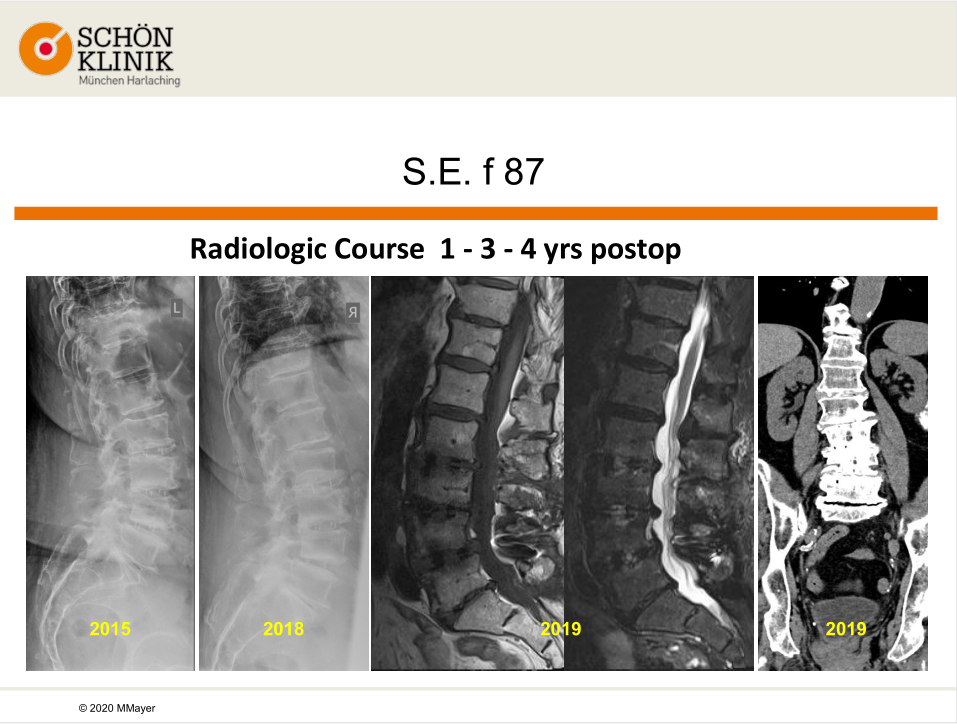
Came back to the case, Prof. Mayer said that the patient’s back pain was getting worse, and conservative treatment was no longer applicable. Then he finalized the treatment by addressing a MIS discectomy on L3-4. At the same time, for stabilisation, he performed L2-5 OLIF with the use of Oracle and BMP.
The patient showed no complications and she could walk stably after 7 days hospitalization. What’s more, the patient’s leg pain was completely gone and her back pain was significantly improved, which excused the necessity of further rehabilitation. In 2019, Prof. Mayer paid a visit to the patient and knew that she had slight occasional back pain but no radicular symptoms, and she could walk 2-3 km and stand for more than 30 minutes without pain. The imaging result also showed that the patient had recovered well.
Prof. Mayer stressed that surgical indications shall be determined in light of the patient’s clinical symptoms; the surgery performance would rather be thought of when the clinical symptoms were severe or progressed; and the surgical solutions shall be determined after considering the risks and benefits. More importantly, a patient-specific surgical solutions shall be made on the basis of the patient’s clinical situation, and shall be finalized after the patient and the family fully understood the given information that relates to the risks and benefits of the surgery.
Pre-operative planning is of vital importance in developing a custom-made surgical solution. Prof. Mayer shared another case he encountered in 2013. The patient was a 75-year-old female who had undergone fusion surgery on L2-5 for degenerative lumbar scoliosis in another hospital. She had progressive back pain and lumbar radiculopathy at right side of L3. And multiple injections treatments, like facets injection and lumbar epidural steroid injections, were no use to ease her pain.
The original plan was first to remove the original implants, to do a posterior release, then to do MINI-ALIF of L5-S1 and OLIF with correction of L1-2-3-4-5 , and then to implant a posterior instrumentation. However, when doing the OLIF approach, he encountered an accident that resulted in an injury of abdominal aorta at L3-4 of the patient. Then a vascular surgeon was called in to handle the situation. A week later, Prof. Mayer proceeded the surgical solution. He did a posterior instrumentation and TLIF on L1-2-3-4 for the patient. 5 years after the surgery, the patient was satisfied with the result, except for occasional sacroiliac joint pain. In the end of the case, Prof. Mayer shared his detailed analysis of the cause of aorta injury and discussed how to avoid this kind of accident in the future.
The Prof. Mayer stressed that it would also influence the planning and execution of a surgical solution if the surgical complications occur.
Normally, the aorta is located at the front side of the lumbar and will shift as the level gets lower in the surgery. It may bring risks for patients with degenerative scoliosis if a change in position of abdominal aorta or a slight retraction of muscles.
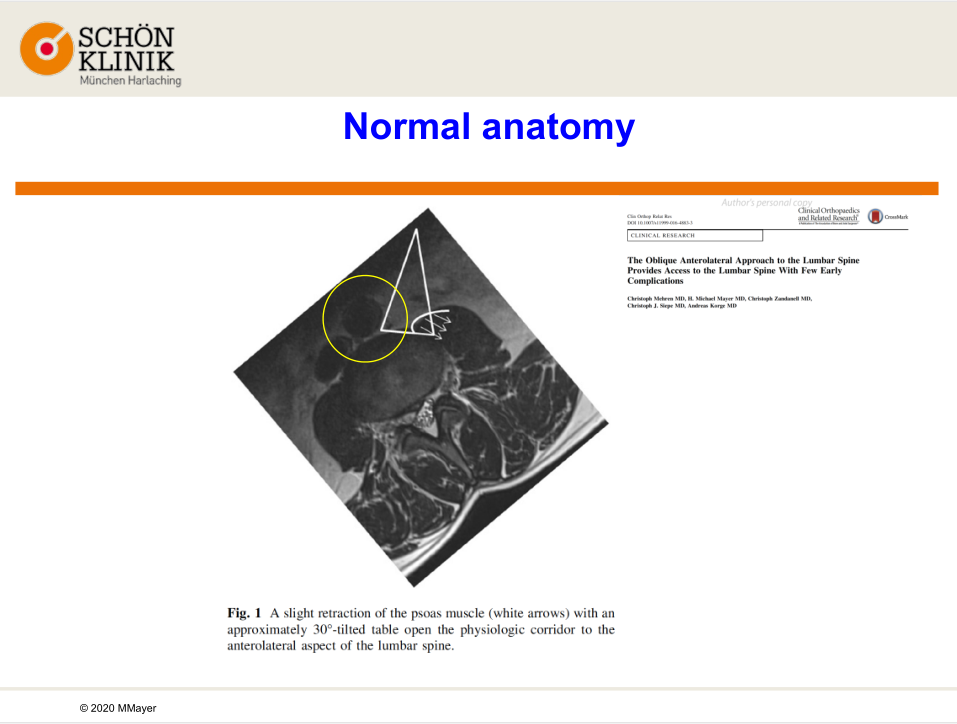
Normally there is a 30° tilted angle between the abdominal aorta in front of the lumbar and the muscle, which is the surgical part for incision. However, in the case the patient’s moving aorta just blocked the part for incision.
Take-home message from this case indicates that it is necessay for a considerate evaluation of the image before surgery to circumvent severe complications and achieve satisfying result.
Prof. Mayer concluded that factors such as the rotation of the abdominal aorta, access provided by the slight retraction of the psoas muscle as well as patient’s informed consent about surgical risks shall be taken into consideration when performing OLIF for treating degenerative lumbar scoliosis.
In the case of degenerative scoliosis with spinal stenosis, Prof. Mayer also explained in detail when and how decompression alone should be performed.
Decompression alone is available for elder patients with underlying diseases if their dominant symptoms at lower extremities and low back pain can be controlled by conservative treatment. Or patients who have rigid deformity, sagittal balance and no evident imbalance are also suitable for decompression alone.
However, Prof. Mayer said there are pitfalls to simply use decompression alone, and showed us how to avoid those pitfalls by sharing case 3 in his study.
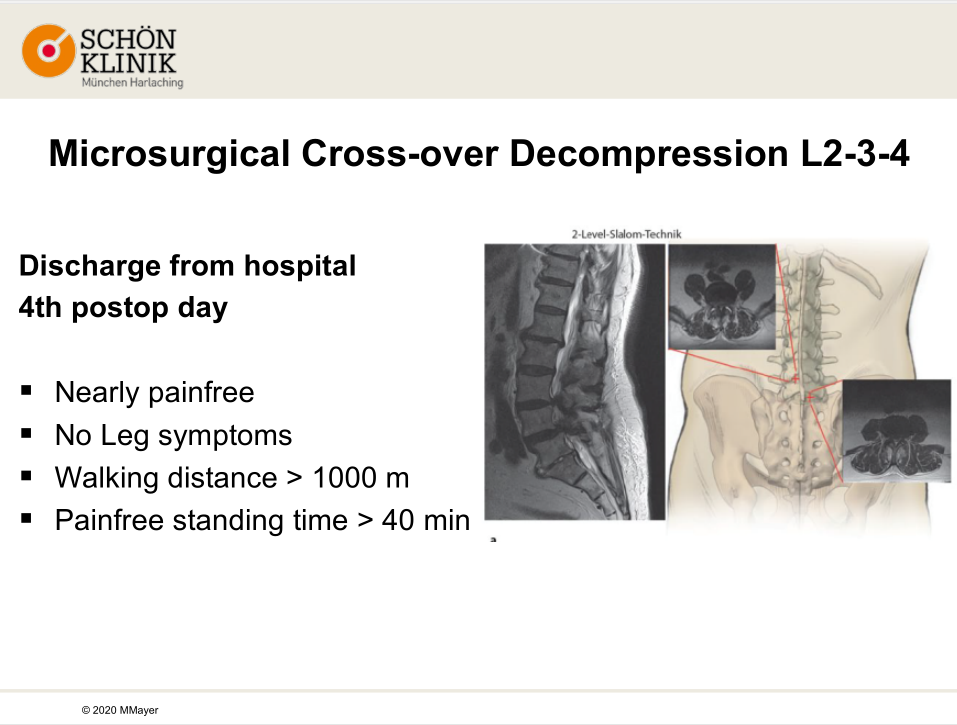
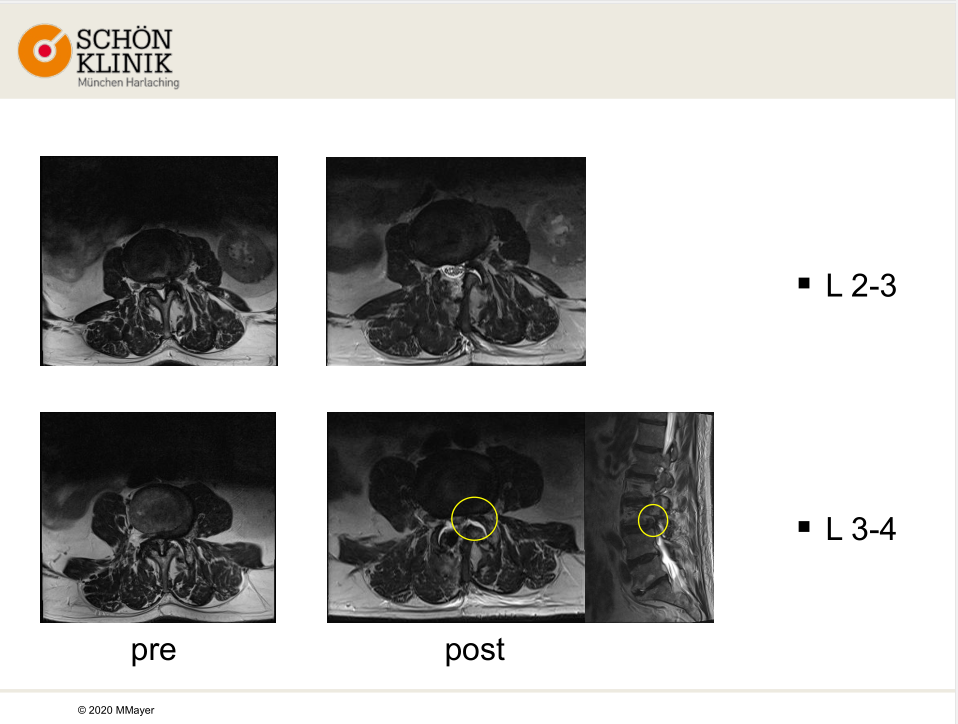
In case 3, this 75-year-old male patient had no relevant back pain but had neurological claudication for two years. He could only walk less than 100 m and stand for 10 minutes painfree. He also felt occasional load dependent pain on L3-L4 in left side The clinical findings of the patient were 1) Loss of lumbar lordosis, 2) Finger-floor distance 30 cm, 3) Straight leg raising test pos. left side at 80° ( L4 Pain), 4) No neurologic deficits. The MRI imaging showed there were severe stenosis on L2-3 and on left side of L3-4. Since conservative treatment was not successful and the patient had no back pain, Prof. Mayer decided to do decompression method alone on L2-3-4 without stabilisation.
After the microsurgical cross-over decompression on L2-3-4, the patient discharged from the hospital. He had no leg pain and could walk more than 1000m and stand for 40 minutes painfree. It was a successful operation.
The MRI scan showed the spinal canal L2-3 was improved, while L3-4 was not sufficiently decompressed which was considered to be responsible for the shoot pain.
So he decided to do re-decompression on L3-4 from left side and do foraminal decompression on L3-4 from left side, but created minimal improvement to the patient. From the new MRI scan, he found occult dural tear on L2-3 and entrapment of L3 rootlets in facet joint space on L2-3, which caused the shooting pain. Based on new MRI result, he did 360° fusion (anterior-posterior) on L3-4, reposition of rootlets L2-3 in left sided and dura-repair on L2-3. The four month postop result showed the patient had no pain or motor deficits. He could walk more than 5km and stand for more than 1 hour without feeling pain.
From case 3, Prof. Mayer concluded that when it comes to degenerative lumbar scoliosis, fusion is an acceptable outcome if back pain is dominant, but there is not much evidence to support this conclusion. When do the fusion, the complication rate is up to 70% in older patients, so as the mortality rate increases significantly. And the reoperation rate also reaches to 11.9-27.4% in 3-5 years.
In the end of his speech, Prof. Mayer stressed that when dealing with degenerative lumbar scoliosis, a doctor should design a personalized surgery solution based on the patient's clinical situation, and that it is better to choose MIS techniques for fusion and decompression. He also stressed that if leg symptoms are dominant, do MIS decompression alone is a rather good choose.
After Prof. Mayer’s speech, Dr. Tian Zhen from The Fourth People’s Hospital of Guiyang gave a presentation about spine infection, titled “Pyogenic Vertebral Osteomyelitis”

Dr. Tian Zhen shared two cases of septic spinal infections. One of the patient had spinal stenosis on L4-S1, treated with decompression + internal fixation. But severe back pain occurred after 6-8 weeks of the surgery. From the postoperative imaging, it turned out to be a loosing on L5. The results of tissue culture and hemoculture were all positive. During his hospitalization, the patient received an empiric antibiotic treatment with ceftriaxone and levofloxacin, but experienced a serological data fluctuation (include CRP, ESR). Finally, Dr. Tian Zhen changed to treat the patient with cefazolin sodium and levofloxacin, which brought the level of CRP and ESR back to normal. After discharge, the patient received another treatment by taking rifampicin and levofloxacin, and doing elastic external fixation at the same time. One month later the patient had complete pain relief.
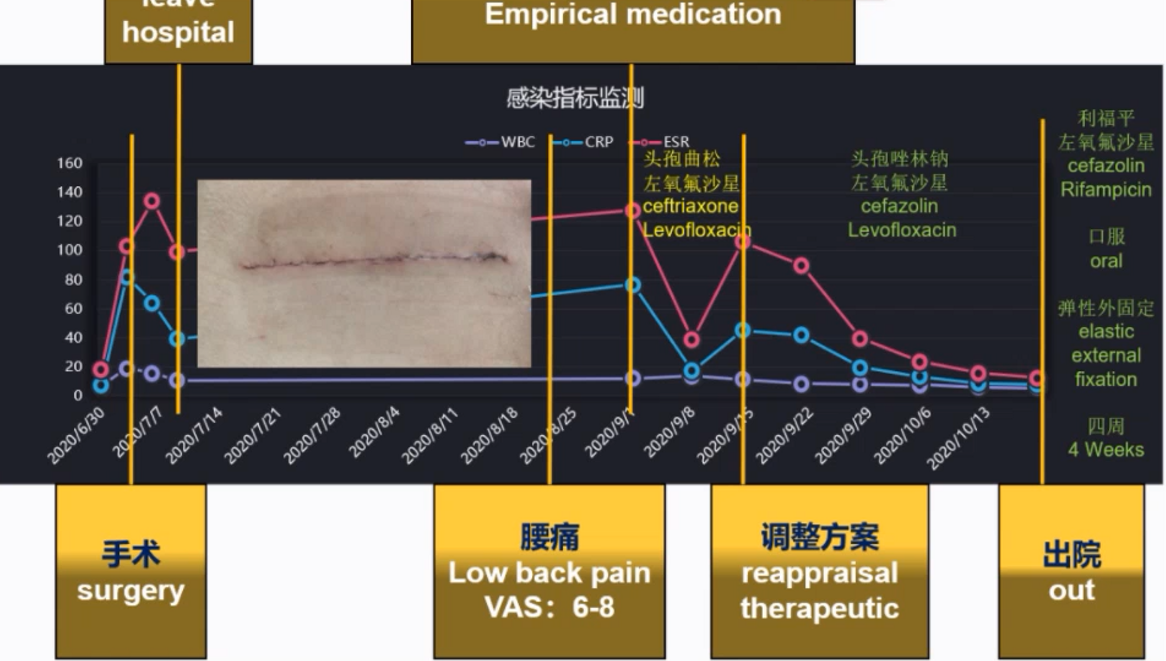
Dr. Tian Zhen concluded that the symptoms of spinal infection are atypical because some patients may have a low level of CRP without fever but still of spinal infection. In terms of spinal infection, Dr. Tian Zhen gave many valuable suggestions, for example, MRI or 18F-FDG-PET/CT is preferred for imaging examination, blood culture or biopsy provides useful information both etiologically and pathologically, an assistance from a pharmacist is required when selecting an antibacterial drugs with strong permeability in the bone and antibacterial drugs should be used with caution before etiological evidence is obtained.
Prof. Mayer thanked Dr. Tian Zhen for his sharing of two different but very important cases which presented the importance of being prudent and careful for a doctor before the diagnosis and surgery solution are made. Spinal infection is a very vital factor to be considered when it comes to an elderly patients. Because of that, preoperative examinations, like MRI, bone scan, and soft tissue biopsy matter a lot in making correct diagnosis and later treatment. During treatment, antibacterial drugs should be used long enough after the decline in the serological data.
Dr. Feng MingXing, Deputy Chief Physician, shared a case of a patient with lumbar spinal stenosis and degenerative scoliosis, emphasizing that the choice of fusion level of lumbar spinal canal stenosis with degenerative scoliosis should be considered carefully, and that the cause of the complication should be promptly identified and treated as soon as possible to minimize the adverse consequences of the complication.
Prof. Mayer greatly agreed with Dr. Feng's approach of doing both decompression and fusion on the patient. Because on one hand the patient’s leg and back pain could be eased, on the other hand the patient is only in his fifties and will have further degenerative scoliosis in the next decades. Prof. Mayer also discussed with Dr. Feng the factors and risks associated with the development of local hematomas and spinal canal hematomas after surgery.
Another case of lumbar spinal stenosis was presented by Dr. Zhang Yang, Deputy Chief Physician. The patient had an immediate pain relief on left anterior thigh after receiving an injection treatment that came with lidocaine and prednisolone on the nerve of L2-3. The data of VAS before and after the operation on left leg was 6 verse 2. The patient still complained about the pain and numbness of the left leg. Then Dr. Zhang Yang decided to carry a combined surgical solution with TLIF decompression+fusion on left side of L2-3 and decompression on L4-5 to relieve much of the leg and back pain.

Prof. Mayer discussed with Dr. Zhang Yang about the reason of the patient’s pain on the left calf.
For this case, Prof. Mayer stated that he would opt for PLIF on L2-3 because the patient's lumbar disc was large and bulging posteriorly, so extensive decompression was recommended. But Prof. Mayer also agreed with Dr. Zhang's approach because the patient recovered well after the surgery. To answer Dr. Zhang's question, “whether he would be concerned about accelerated degeneration on L3-4 if an L2-5 fusion was done on L2-5”, Prof. Mayer’s answer was yes. Because it increased the pressure on the spine. He emphasized that the surgery should be done for restoring as much of the patient's physiologic curvature as possible and that placing the fusion from the front could achieve better result.
Prof. Mayer gave a closing speech about this video conference saying that he felt so honored to have this opportunity to join this video conference. And although he had a different surgical opinion on the cases, he felt so blessed to get inspiration from the cases.
At the end, on behalf of the hospital, Dr. Xiao Jie, Director of Spine Surgery of The Fourth People’s Hospital of Guiyang, expressed his thankfulness to Prof. Mayer for his valuable sharing and invited him to visit Guizhou, China for further face-to-face academic exchange in the future.
