-
News & Events

For this episode, Gloryren has the honor to invite Prof. Boriani, World-class Master for Spinal Tumor who had developed WBB staging system, Director of Spinal Teaching Program and Head of Spine Tumor Surgery of the GSpine4 Spine Surgery Division IRCCS Istituto Ortopedico Galeazzi Milan. In the interview. Prof. Boriani shared with us his stories of early life, the development and application of the WBB staging system and his experience in performing en bloc resection, ect.

1. How did you become interested in taking up spine tumors as your carrier when most of the spine surgeons avoid managing this condition? What made to take such an interest in this field?
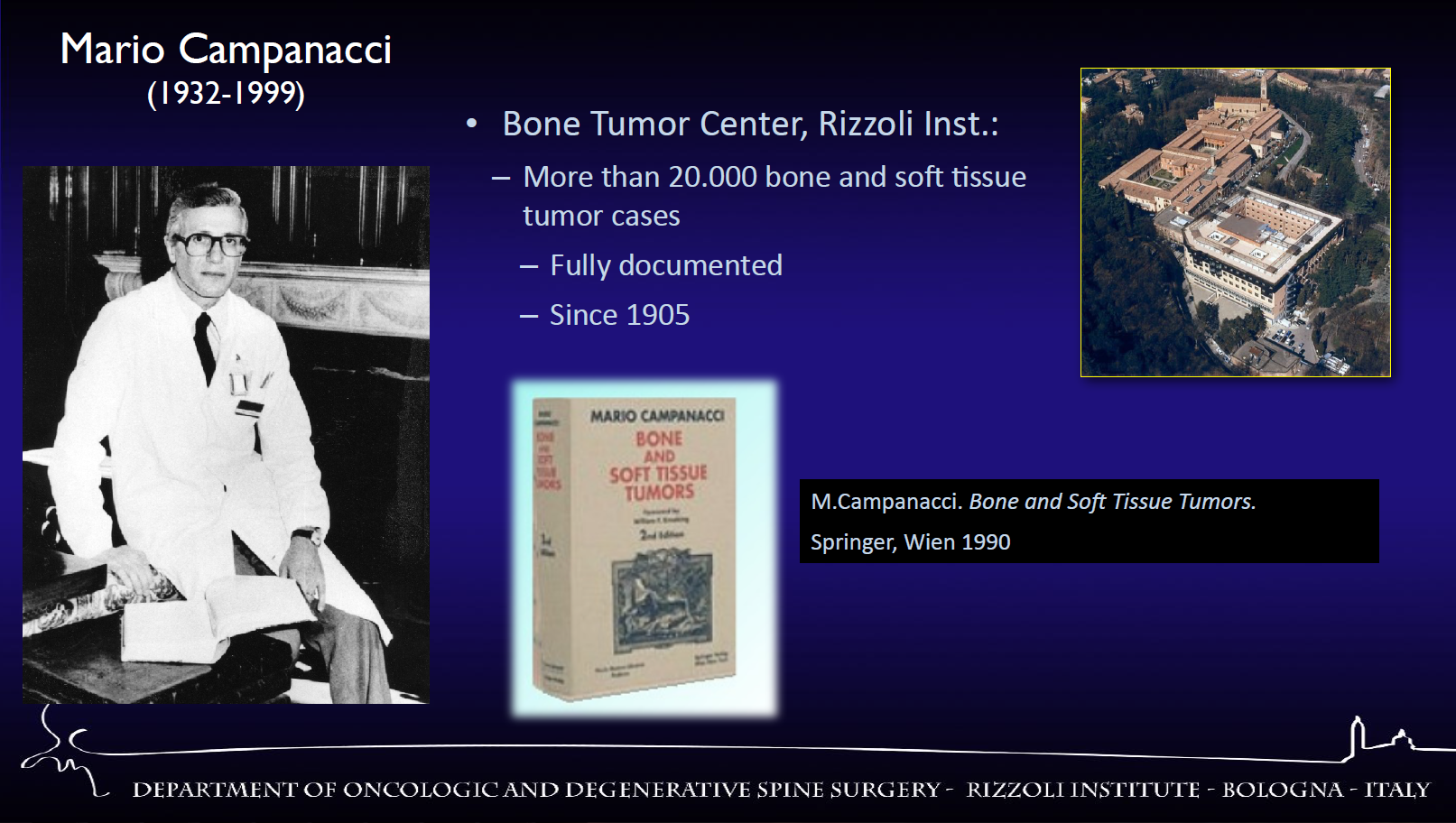
This is a very interesting question as it has me to go back to the beginning of my activity. I was born and I studied in Bologna, which is the site where the most important institution of Orthopedics was founded in 1896. It is Istituto Ortopedico Rizzoli. This center has been and is still the most important referral center for bone tumors. And more than 20,000 cases have been recorded since 1905.
So I entered in this institution as a student in 1974, and since that time I had the opportunity to have Prof. Campanacci as a mentor. Prof. Campanacci was an orthopedic surgeon but also a pathologist. And he was interesting in bone tumors and he wrote one of the most important textbooks on this topic.
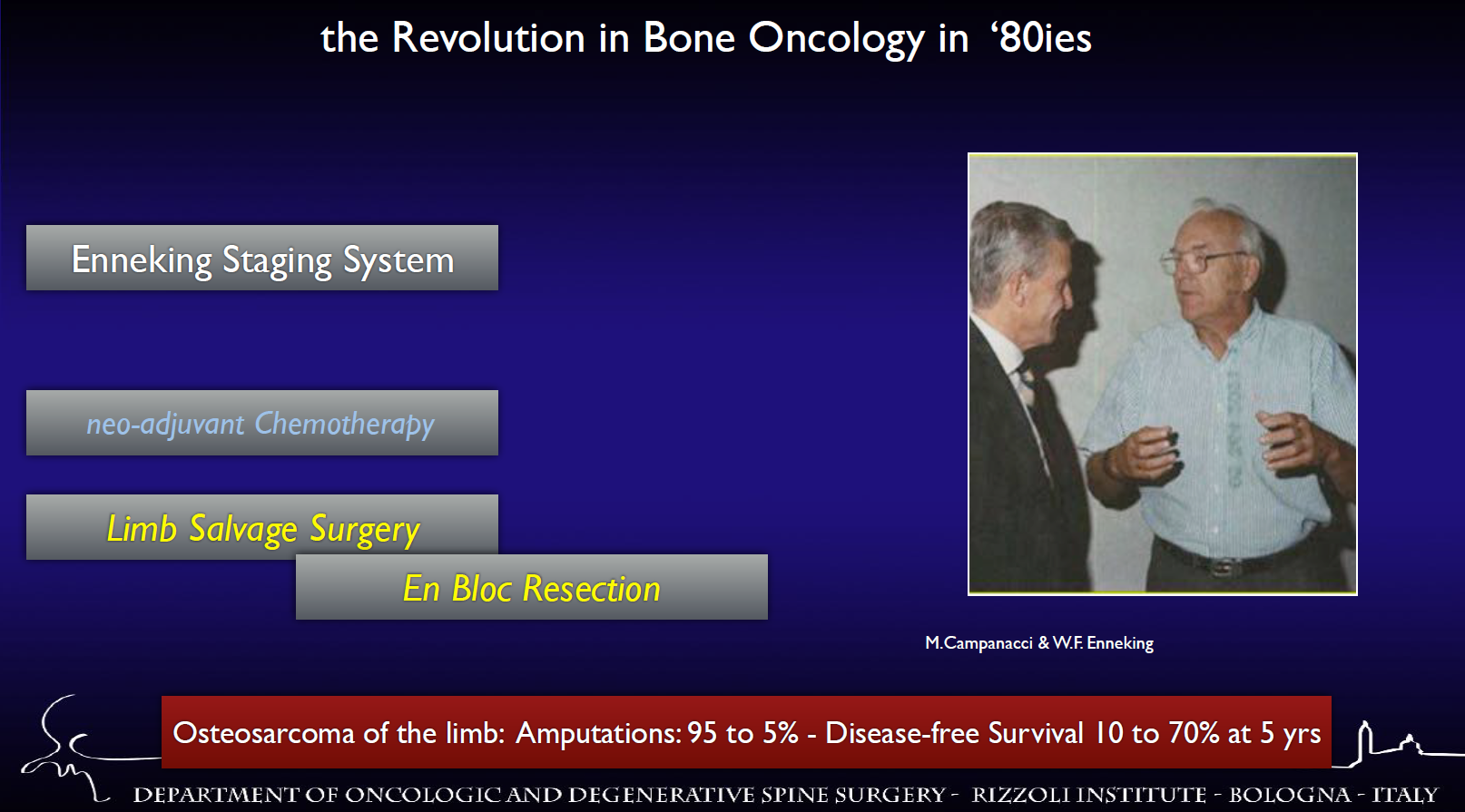
Prof. Campanacci was involved in the great evolution in the treatment of bone oncology together with Enneking. And the result of the combination of these expertise brought to great successes. For example, the reduction of amputation rate in osteosarcoma of the limb and the disease-free survival improved from 10% to 70%.
So my life changed completely the day which I think was in the spring of 1984 when Prof. Campanacci invited me in his office, and told me, “Stefano, I think that we should study if the criteria accepted for bone and soft tissue tumor of the limb are applicable to bone tumor of the spine.” This was the day which changed all my life, and since that day I started to work on this subject. And today I have collected more than 2,000 cases and dedicated all my life to working on this subject.
2. Is there anyone who affects you most in your study or professional career? If so, who’s he (she) and how did he (she) affect you?
This is also a very important question as it includes not only professional point but also some points which concern my intimate life.
As you know what is important for a doctor is to have a mentor. My mentor was Prof. Campanacci. What is important, the important role of a mentor is that the sentences and the leading idea that are in the mind remain all the life. For example, he always reminded that the pathway for successful medical care is the patient-centered activity, meritocracy, team approach and international relationships.
These are generally leading ideas that remain in the mind all over my life. For example, team approach for bone tumor in the spine includes these points: that should be a multidisciplinary decision-making process with careful studies, multidisciplinary treatment; the surgical plan should be following to oncological principles; and neurological function and spine alignment and stability must be preserved.
The role of a mentor is to remind always that common sense is very wise and this is a sentence that I always remind every time I have to decide something. It’s very simple, “when you have to decide a treatment, you should avoid a too shy treatment, unable to get the result, but avoid also a too aggressive treatment, exposing the patient to unnecessary morbidity... ” So my mentor pushed me to study this activity and he rested also in my mind with this sentence and this idea.
There is something that should help everyday. For example, the music which is helpful to find concentration and stimulate creativity. I like so much, for example, Richard Wagner, which was a German composer.
But it is also very useful to have home somebody who is tolerating, that is thinking the patient everyday and I think planning surgery. It is very important to have a family, the warmth of a family is very helpful to maintain concentration and to work at the best for the patient care. So I must acknowledge to my wife, Loredana, to my cats, to help me in every day rest and in the best to find the concentration for my difficult job.
3. During the past time, the treatment for spine tumor was not so specific, so how did you make some breakthroughs to solve this problem?
So you are fully right. When Prof. Campanacci asked me to find the best solution for the treatment of tumor, this was what we can do for any kind of tumor, just intralesional excision was done with very bad result. There was no different activity, all the tumors both benign and malignant had to be treated by the same intralesional approach, which was disastrous for malignant tumors.
In the early 80s, there were some attempts to perform en bloc resection, but it was not performed according to oncological appropriateness. So the result was not so satisfactory as the patient had a local recurrence and died.
The new strategy was to apply to the spine the same criteria used for the limb. And the first point is the concept of “en bloc resection” which means to remove the tumor together with the continuous shell of healthy tissue, which is so-called the margin. And the thickness of the healthy tissue that we can leave around the tumor must qualify the oncological validity of the procedure. But for anatomical reason, it is very difficult to perform en bloc section in the tumor of the spine due to the anatomical problems.
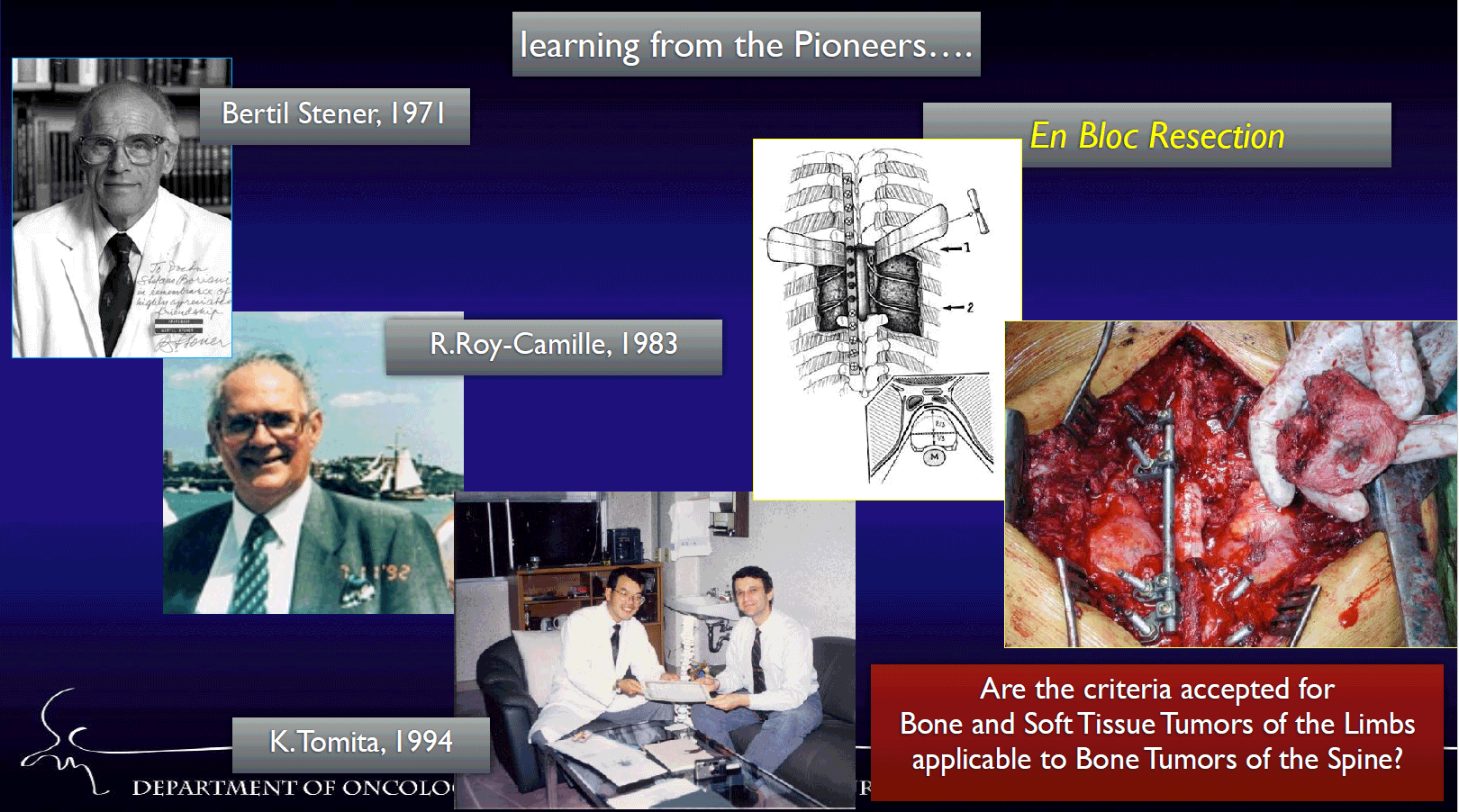
So I decided to start learning from the pioneers of this surgery. The first who applied to the spine oncological criteria was Bertil Stener, a Swedish surgeon who performed two en bloc sections in the spine in 1971. Later on R.Roy-Camille and K.Tomita tried to find the surgical technique able to resect en bloc vertebrae. So I started working with these great pioneers in order to find my way to perform en bloc resection in the spine.
But the real key to understand which is the best treatment is staging, is to decide which is the best kind of resection according to the aggressiveness of the tumor. This was the proposal of Enneking Staging System and based on the staging, it was to be decided the margin. So one of my first relevant papers was the application of the spine of the Enneking Staging System. We published this paper in 1997 and this is the basis to decide the best treatment in bone tumors in the spine.
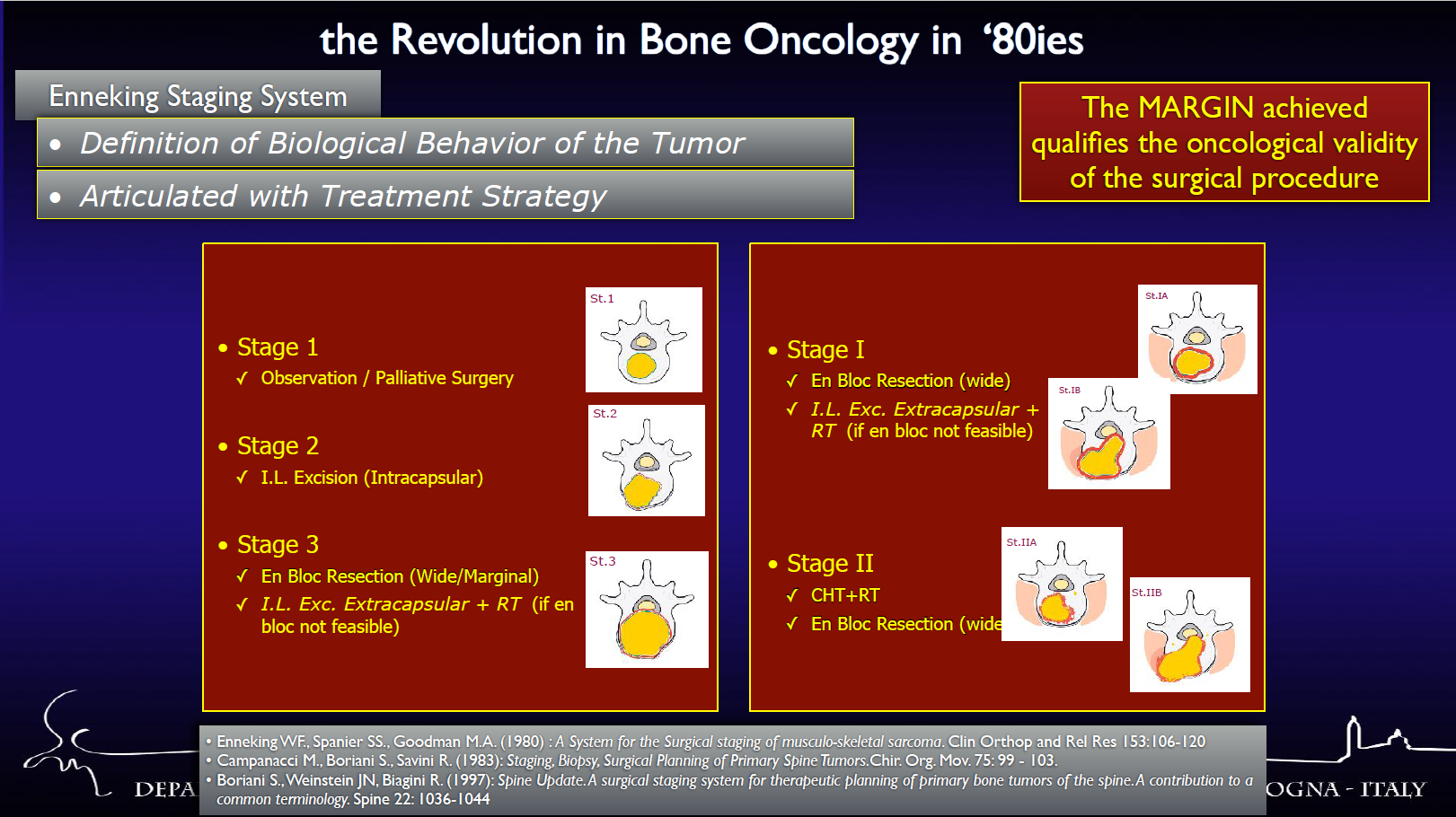
So by understanding and classifying the biological behavior of the tumor, we can decide the treatment strategy. I think this was an important contribution to understanding how to treat this tumor. So this is the way we are following and since this point we started with our job.
4. It’s known that you did an En-bloc surgery for treating spine tumor at the age of 39, what kind of impact or influence this kind of approach has brought to the treatment of spine tumor?
We started performing en bloc resection in a low grade malignant tumor, for example, a chordoma. It is a chordoma on L3, which we did the en bloc resection for the first time. It was done on October 25 in 1991 and I was at the age of 39. I arrived to this point after promoting the staging system by Enneking and after going all around the world to see the other people that performed this surgery.
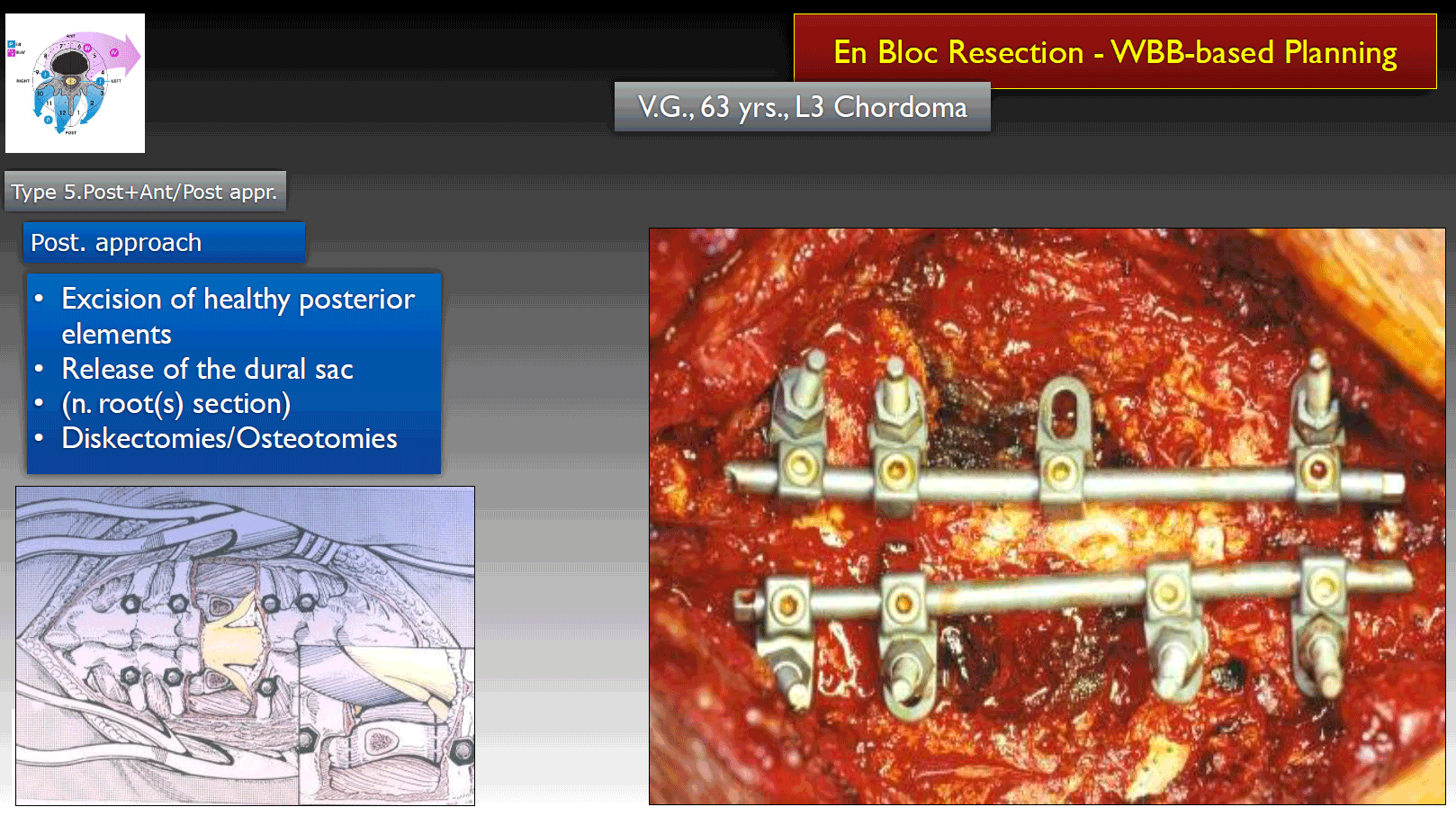
An old style of fixation performed in the first en bloc resection surgery
So we concluded the en bloc resection by removing the tumor with a good margin. It was a very successful surgery that the patient survived without any problems for 8 years and died for another disease.
We did another case a few months later with more difficult chordoma on L5. We had to achieve a full en bloc resection, we did perform three approaches, first anterior and then posterior and we concluded with another anterior approach. This was a very successful surgery with good margin all around the chordoma. The patient is surviving after 24 years without any evidence of disease. This is a good demonstration that if we have applied staging and the correct oncological treatment we can achieve excellent result. So the important point is the role of margin as our further studies.
As indicated that if we have applied Enneking appropriate surgery, we have 7% of local recurrence and if the Enneking staging system is not applied, the local recurrence rate is about 10 times higher.
This was a study from Prof. Fisher, which was demonstrating the same. This study promoted and confirmed that Enneking appropriate treatment is associated with the statistically significant result on local recurrence rate and on mortality.
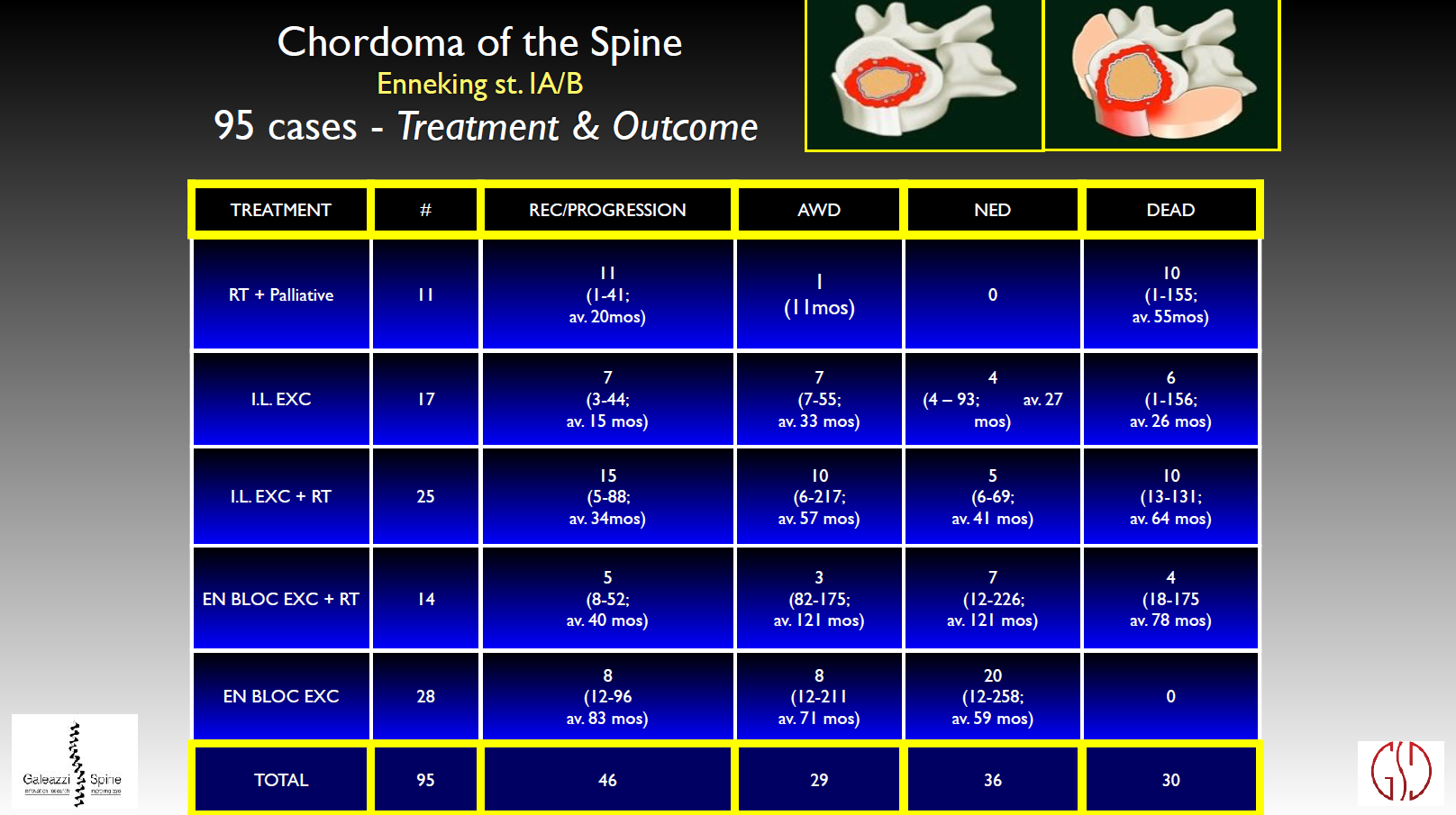
Later we performed several studies on single histology. For example, this was the result of 95 cases of chordoma on the spine. The result of the study is that en bloc resection is associated with the best result but the local recurrence rate is still not fully satisfactory. The results are better with chondrosarcoma where en bloc resection with the good margin is always associated with excellent local control and survival of the patient.
So my contribution to the literature was not only on promoting the surgical technique, but also understanding the revolution in the times of this technique.
Our conclusion is that if in a case of chordoma like this, if it is performed intralesional excision instead of en bloc resection. The result will be very bad. And the intralesional treatment which doesn’t respect the oncological principles will end in local recurrence. And the real problem is that after the first local recurrence, even if we perform en bloc resection we can not save the patient’s life. The local recurrence was treated by en bloc resection, but even en bloc resection could not save the patient as more local recurrence and the death followed with in this case.
So a sentence that I always repeat is that the first treatment is the one would decide the patient survival and the patient evolution. So those who want to start to work on tumors have the great responsibility, as the first decision is the one will affect the final prognosis.
5. Nowadays, WBB classification created together by you and your colleagues is widely used in today’s spine tumor treatment, and how it has revolutionized the management of vertebral column tumors? And some new and uncertain cases of spine tumor may appear in the future, in this regards, is it necessary to perfect the existing WBB classification in case of the new cases? How would you to perfect it?
First of all, let me introduce you how we promoted and developed the idea of WBB. It’s very important to decide and stage the biological behavior of the tumor by Enneking Staging System. And what is needed for staging and planning this kind of surgery is to share with other doctors’ ideas and knowledge of the tumor extension. So in other words, we found the need to have a system to stage the anatomical tumor extension in order to decide the treatment.
Meeting Weinstein JN became the key
Weinstein JN is the chief editor of the most important journal of spine. And till that time he was very interested in staging this lesion. At the early day he proposed a very simple kind of staging. We had a lot of discussion together and revised his system.
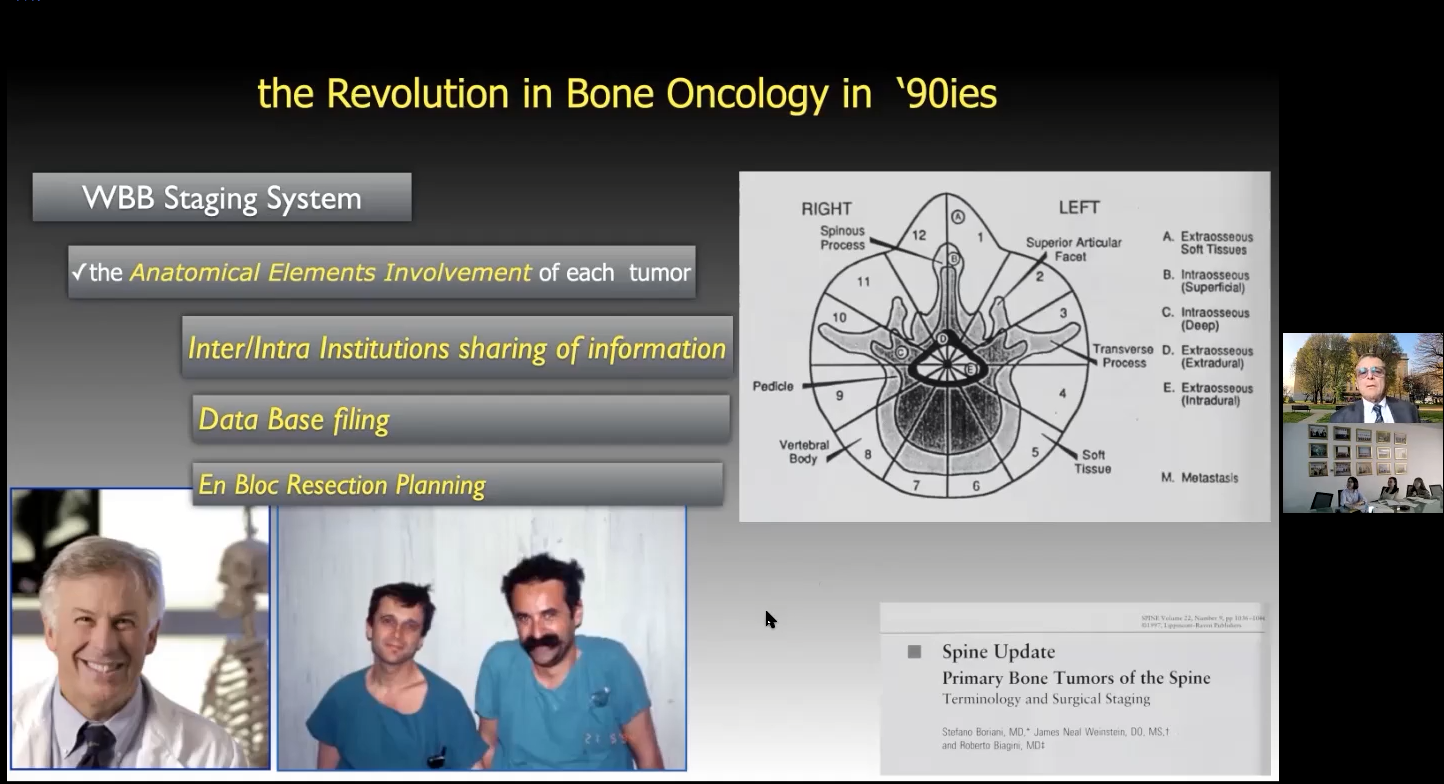
Weinstein, Boriani, and Biagini were young co-workers at that time.
The idea of this staging system is to share information inside the institution among professionals to file data base and to plan en bloc resection.
The reliability is an important character of classification
The reliability is the most important character of classification as everybody should be able to use it, and obviously, if it is not possible, the classification is not helpful. We had revised the WBB together with a multidisciplinary group of experts of spine tumor. We submitted this revised pattern to an analysis of reliability. And we have achieved that 75% of agreement in inter-rater reliability and 89% in intra-rater reliability which are excellent result.
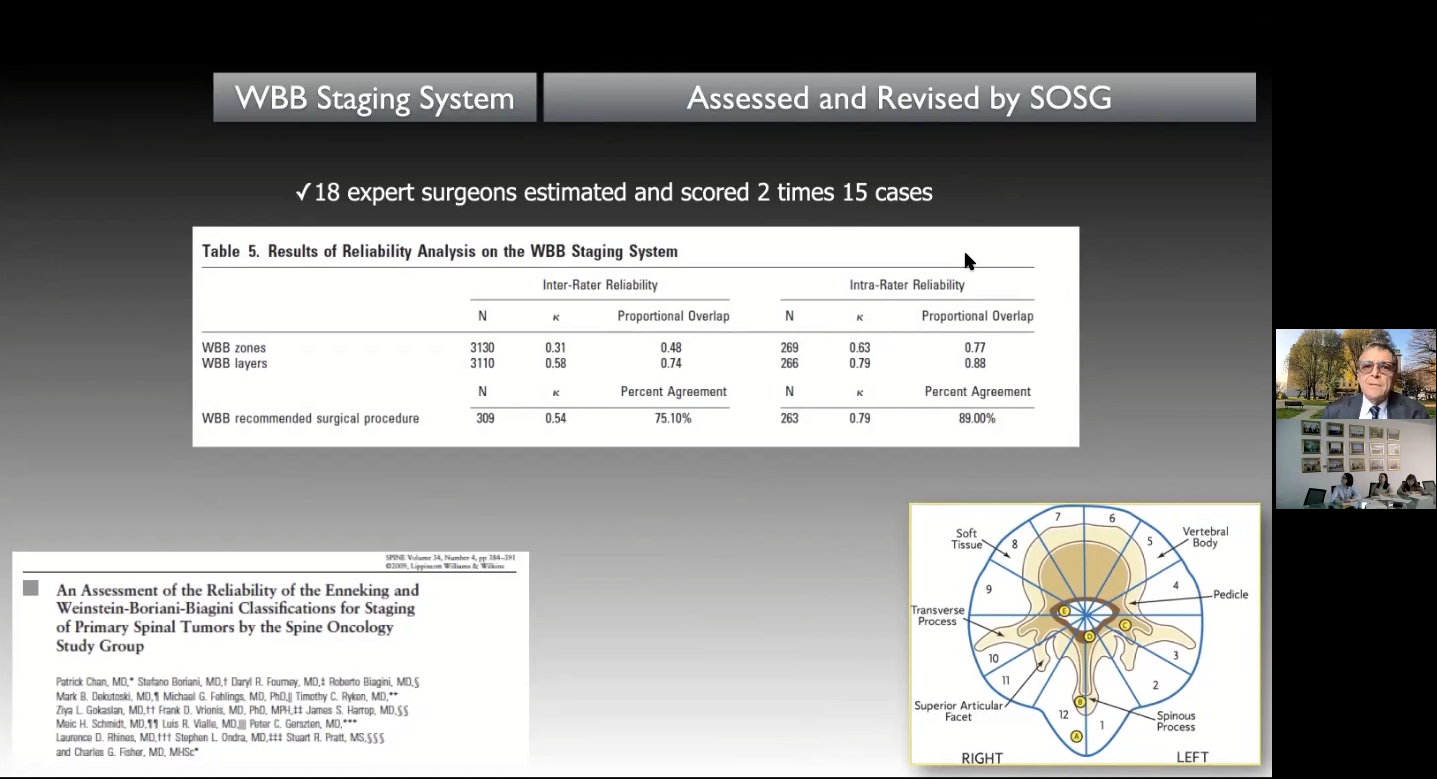
The revised WBB classification and its reliability analysis
And one of my last contribution in the literature is to use this new WBB for planning the en bloc resection. So based on the WBB, we can select seven different kind of en bloc resection according to the tumor extension.
6. Could you please share one case that you think as the most challenging and impressive one?
There are many challenging cases, here I would like to show you a case of cervical chondrosarcoma, to show you what we called Type 3a en bloc resection. First we performed an anterior approach to release the tumor completely, leaving a margin of healthy tissue over it, then created a groove in the vertebrate body arriving into the canal, and leaved a plate for anterior stabilization. After that we turned the patient and performed a posterior approach. We found the lamina from one side and the other side we went all around the tumor and reached the anterior release. At this point, we did a laminectomy and ligated the dura sac and cut C5 and C6 nerve roots so as to enter into the tumor. To save a good margin, we had to sacrifice these nerve roots, so we can displace the dural sac and reach the groove that we had performed anterior and then removed en bloc all the tumor with the satisfactory margin. Later we had done a cervical thoracic fusion for the patient. The result is very good as we have a five years follow-up without any evidence of disease.
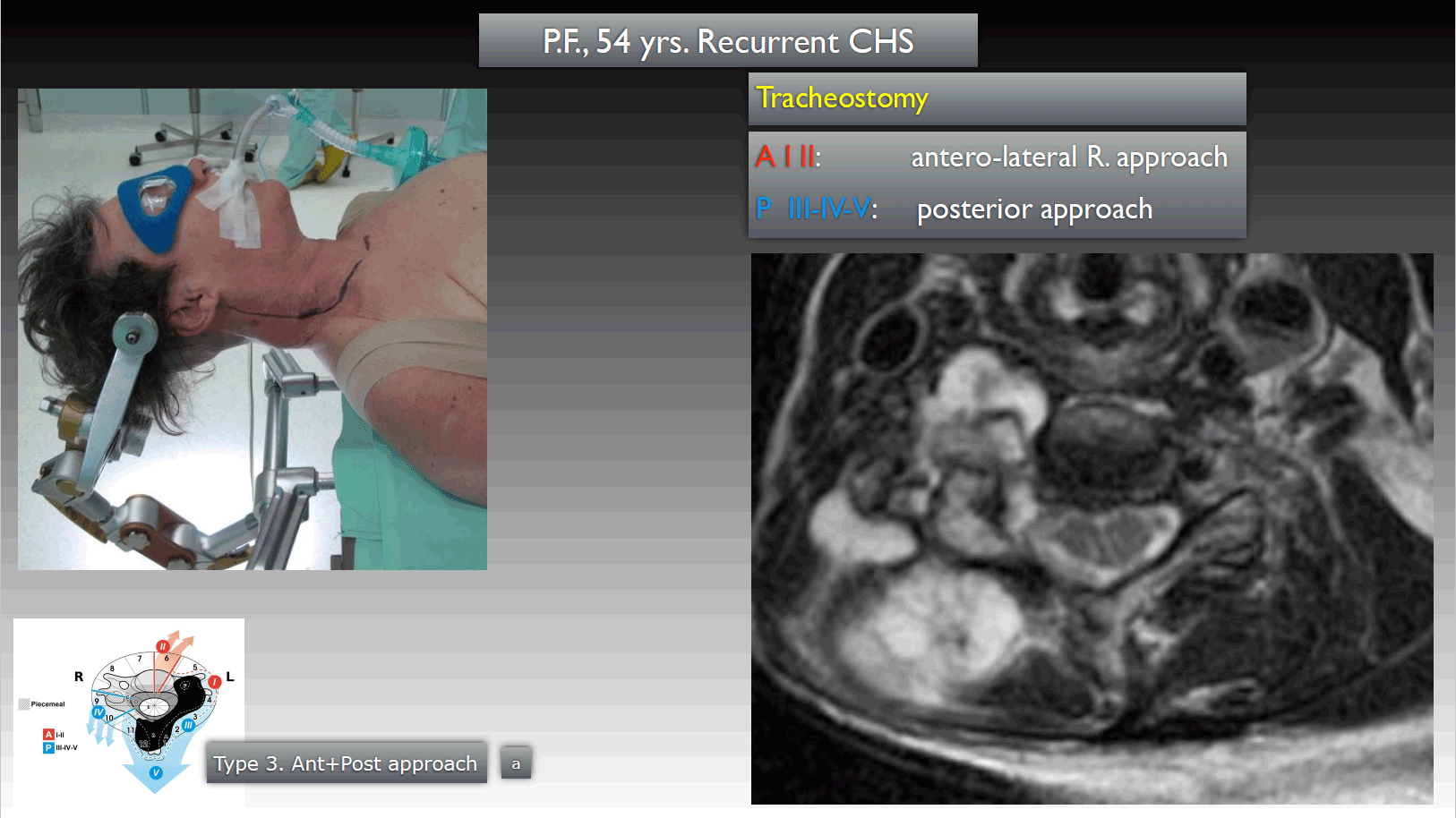
I think this is a good example of application of our surgical technique in performing en bloc resection in bone tumor on the spine.
7. We notice that you have been part of IRCCS Istituto Ortopedico Galeazzi since 2017, and how does this participation help your later study in spine tumor?
Let me talk about the role of multidisciplinary activities in spine tumor. As I think that it’s very important to the expertise of spine surgeon to dedicate to deformities, as we have sometimes problems from a mechanical point of view after en bloc resection.
We did an en bloc resection of two vertebrate. There was a very good fusion and no problems of the tumor, but the patient had the progressive instability and not withstanding several surgical revision that was lost of balance. So we are trying to understand why this happen and the answer is that there are different types of spine even in the normal population and they mostly are divided into four different types. When we have to perform a reconstruction, we have always to think to the individual spine types. At the beginning of my experience in vertebrectomy. We only think to perform circumferential reconstruction anterior and posterior, believing that this was enough.
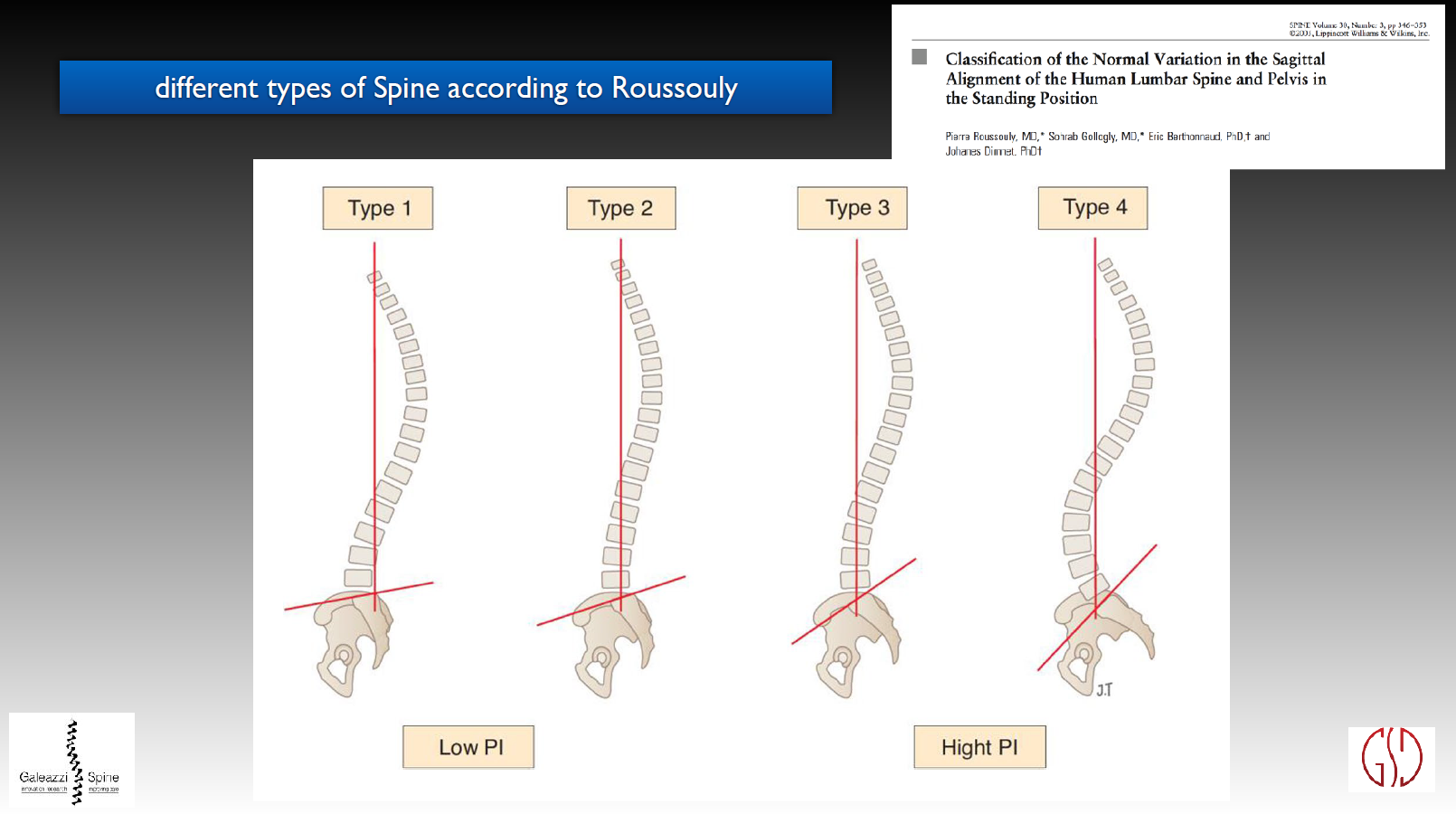
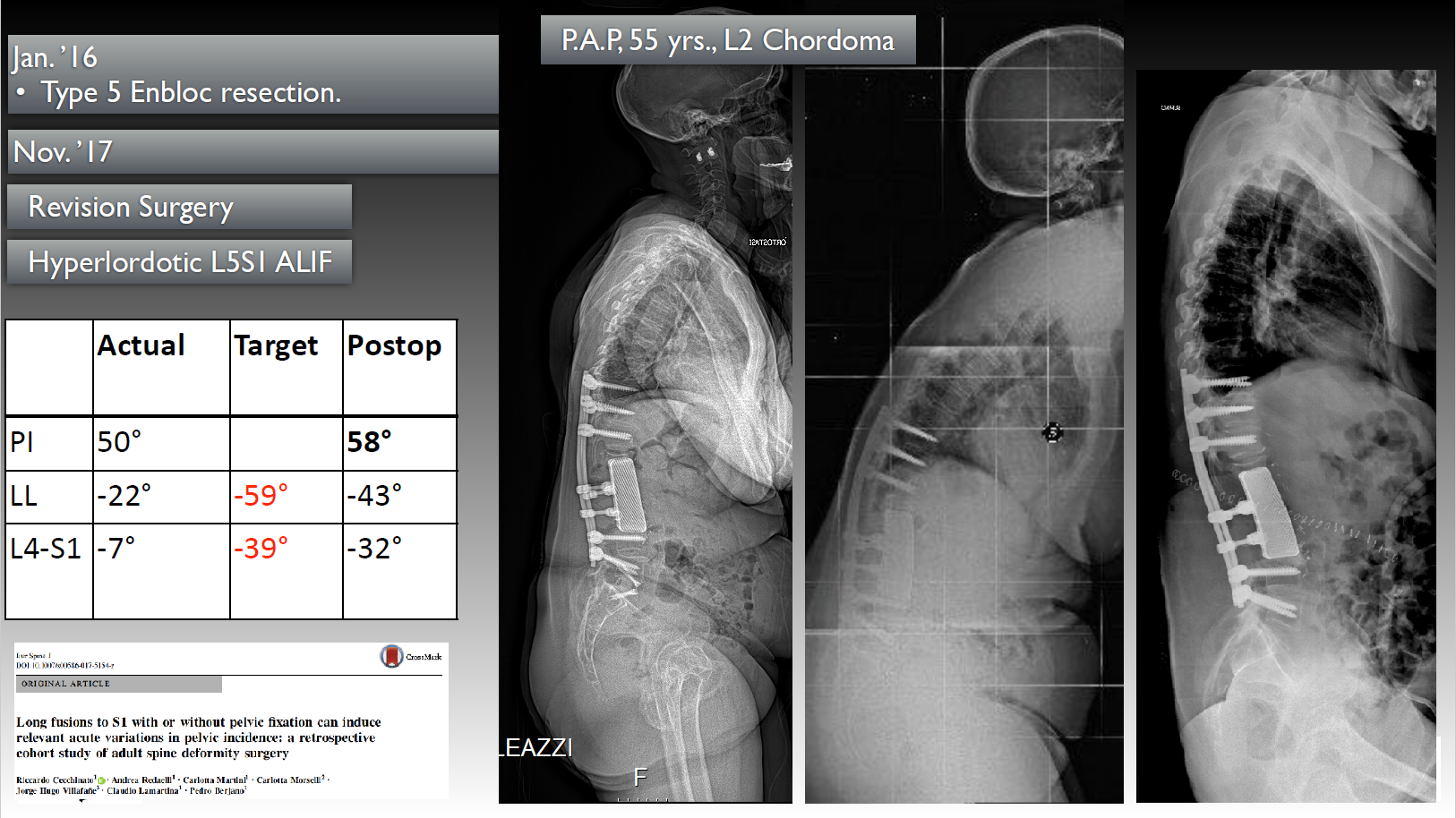
This was a very huge chordoma of L2 that we had to resect it by three different approaches. The first we did the posterior approach separating the dural sac and then we put the patient on the side and removed three vertebrates from anterior approach. The removal of the tumor was with a good margin. So it was good from the oncological point of view. Then we did the 3D reconstruction using anterior 3D printed cage and then the posterior system. But we didn’t realize that there was a very high pelvic incidence. We did a good surgery from the oncological point of view, but not a good surgery from a mechanical point of view. Just anterior and posterior reconstruction is not enough, we must restore the normal spine type.
So now our job is to promote a staging system for considering the right sagittal and coronal alignment for the reconstruction in order to restore the physiological spinal shape. This is the job we are doing now in our spine team.
8. What are your suggestions to the doctors who would like to or have embarked on the field of spine tumor?
Be passionate
My suggestion is to have a passion for the work. This is a very difficult job. And those who want to follow this way, the most important point is passion, to be passionate.
Our patients are very difficult to manage, as they have many problems, and they are very concerned about their selves situation. To save their lives, we have to propose them very difficult surgery with the least intraoperative death, with the least very important functional problems. So it takes a lot of feeling into discussion with the patient.
So those who want to follow this way must consider that in the weekend, the mind will be occupied by thinking which is the best strategy to perform and the best way to communicate with the patient. We have no free time indeed.
9. How to face the failure in spine tumor management?
As the complication is very frequent and really takes you a lot of problems, a lot of thinking and you may lose a lot of your privacy in this. I would like to share a case of chondrosarcoma that operated with a typical procedure I showed you. We had a tear of the dural during the surgery, but we repaired and it seemed that everything went smoothly with en bloc resection and with a good reconstruction. However,
2nd dd post-op: the patient could not move any more his legs. I did perform in the night an emergency decompression, and evacuate haematoma and the motor function was recovered.
7th dd post-op: the patient had hyperpirexia with urinary symptoms. We started anti-biotic treatment.
12th dd post-op: the fever raised up again to 39 degrees and the patient again had an incomplete paraplegia. We did a CT scan and there was a huge collection of liquid around the dural. So we did perform a CT scan guided drainage(200cc), colture, and start a multiple anti-biotic treatment. But not withstanding the treatment, the collection, and the fever was increasing, so we did a new debridement anterior and posterior and replaced the cage together with gentamicin beads. Again the motor function recovered.
28th dd post-op: there was still a CSF leakage with another incomplete paraplegia, so we had toopen again the wound to put the local anti-biotic with the tobramicin beads and completed the compression again. The motor function recovered.
So finally things were going better, but this patient had three surgical revisions and three months anti-biotic treatment. He had recurrent paraplegia, so he needed six months of rehabilitation program.
4 years post-op: there was no problem with tumor and the patient was able to walk with some imbalance but was able to go back to his activity.
5 years post-op: unfortunately he had the myocardial infartion in June 2013.
8 years post-op: it was surprising that in October 2016, he had the recurrence of local infection and the progressive loss of autonomy, and finally died for heart failure in January 2017.
So I think that this case can describe correctly how heavy is this surgery if you want to perform an oncological appropriate surgery. If there is one complication later on step by step, you could have more complications and finally sometimes even the death of the patient unfortunately.
10. How do you find a balance between daily work and life? Or what kind of hobby do you have when you are off work?
My daily life in the hospital is very difficult. You can save a little bit your life with the music and with the love of your wife, of your children and of the cats. The life is very difficult when there is always thinking of the problems of the patient. So this is a problem that we have to face everyday, we have to study, have to use the passion. We have to accept that we can not leave the problems in the hospital, the problems of the patient come with me, otherwise it is impossible to face these problems.

Prof. Dr. med. Stefano Boriani
Director of Spinal Teaching Program and Head of Spine Tumor Surgery of the GSpine4 Spine Surgery Division IRCCS Istituto Ortopedico Galeazzi Milan (I)
Brief Introduction:
Since 1978, Stefano Boriani had been working as an attending surgeon at Rizzoli Institute in Bologna (I) until 1988, then took over the sub-unit of Oncologic Spine Surgery in the Department of Bone Tumor Surgery as an associate chief physician until 1996. Then charged as Head of the Department of Spine Surgery at Istituto Santa Corona di Pietra Ligure (SV) from April 22nd to September 21st, 1996. He had been working as Head of the Department of Spine Tumor and Degenerative Spine Surgery at Rizzoli Institute in Bologna since September 6th 2009. Currently, he is Director of Spinal Teaching Program and Head of Spine Tumor Surgery of the GSpine4 Spine Surgery Unit.
Major contributions to surgical and scientific interest concerns diagnosis and treatment of spine tumors worldwide recognized are:
• The original staging systems for primary tumors, well known as WBB presented in 1996 and now applied by most spine oncologic surgeons.
• Research and publications of surgical protocol for primary spine tumor.
• Original techniques for primary spine tumor excision.
Memberships:
• 2006-2009: Co-chairman of spine surgery research group
• 2005-2009: Chairman of AO Spine Italian Council
• Past Chairman of the AO Spine Knowledge Forum Tumor and actually Member of the Steering Committee
• Honorary Member of the Spine Societies of Hungary
• Honorary Member of the Spine Societies of Israel
Brief introduction to the Galeazzi Orthopaedic Institute
The Galeazzi Orthopaedic Institute, I.R.C.C.S., founded in 1963 in Milan, is the first Orthopedic Center in Lombardy, Italy. Meanwhile, it is the In 2001, the center was accredited as Scientific Institute for Research, Hospitalization and Health Care by Italian Health Administration (I.R.C.C.S.).
The hospital has developed into a multidisciplinary center that possesses more than 35000 square meters, 364 beds for emergency care, 14 operating rooms and multiple outpatient clinics. The center has 20 different functional units dedicated to orthopaedics, trauma and joint replacement. The center has been known as the largest orthopaedic hospital in Lombardy since 2001, for having 3300 spinal fusion surgeries and 1000 spinal fixation operations every year. Certified by the National Health System (NHS) as the center of excellence in clinical biomedical research, pre-clinical research and teaching activities, the Galeazzi Orthopaedic Institute, I.R.C.C.S. is the medical teaching cooperation base of the University of Milan. The Institute has joined the San Donato Hospital Group in 2000 and, it has since then extended its medical and surgical specialties (in addition to orthopaedic) to include Maxillofacial Surgery, Rheumatology, Plastic Surgery, Physical Medicine, and Neurosurgery, as well as Outpatient Neurology, Cardiology, Endocrinology, Otorhinolaryngology, Dentistry, Vascular Surgery and Dermatology. The institute takes the health and well-being of patients as the first priority, promising to support patients’ right of being treated and taken care of most properly with enthusiasm and determination through series of activities and work to maintain its characteristics of excellence and efficiency in the name of health.
The institute is certified in accordance with UNI EN ISO 9001 for management of health care and scientific research. It had been a member of international orthopedic central association, and certified as one of the most excellent institutions for research in the fields of orthopaedics by 16 countries and 19 institutions, ranking the first of having largest number of knee joint prosthesis in Italy in 2013.

