-
News & Events

From June 14 to 20, Dr. Hartmut Stinus, former President of the German Society for Foot and Ankle Surgery (GFFC), Chief Medical Officer of the German delegation at the Beijing 2022 Winter Paralympics, and Senior Consultant of Foot and Ankle Surgery at the University Medical Center Göttingen, Germany, was invited to visit Foshan Hospital of Traditional Chinese Medicine as an International Visiting Professor. During the five-day academic exchange, Dr. Stinus was actively involved in a wide range of activities, including outpatient consultations, ward rounds, case discussions, surgical guidance, public lectures, and departmental management training, engaging in in-depth, comprehensive interactions with the hospital’s foot and ankle surgery team.
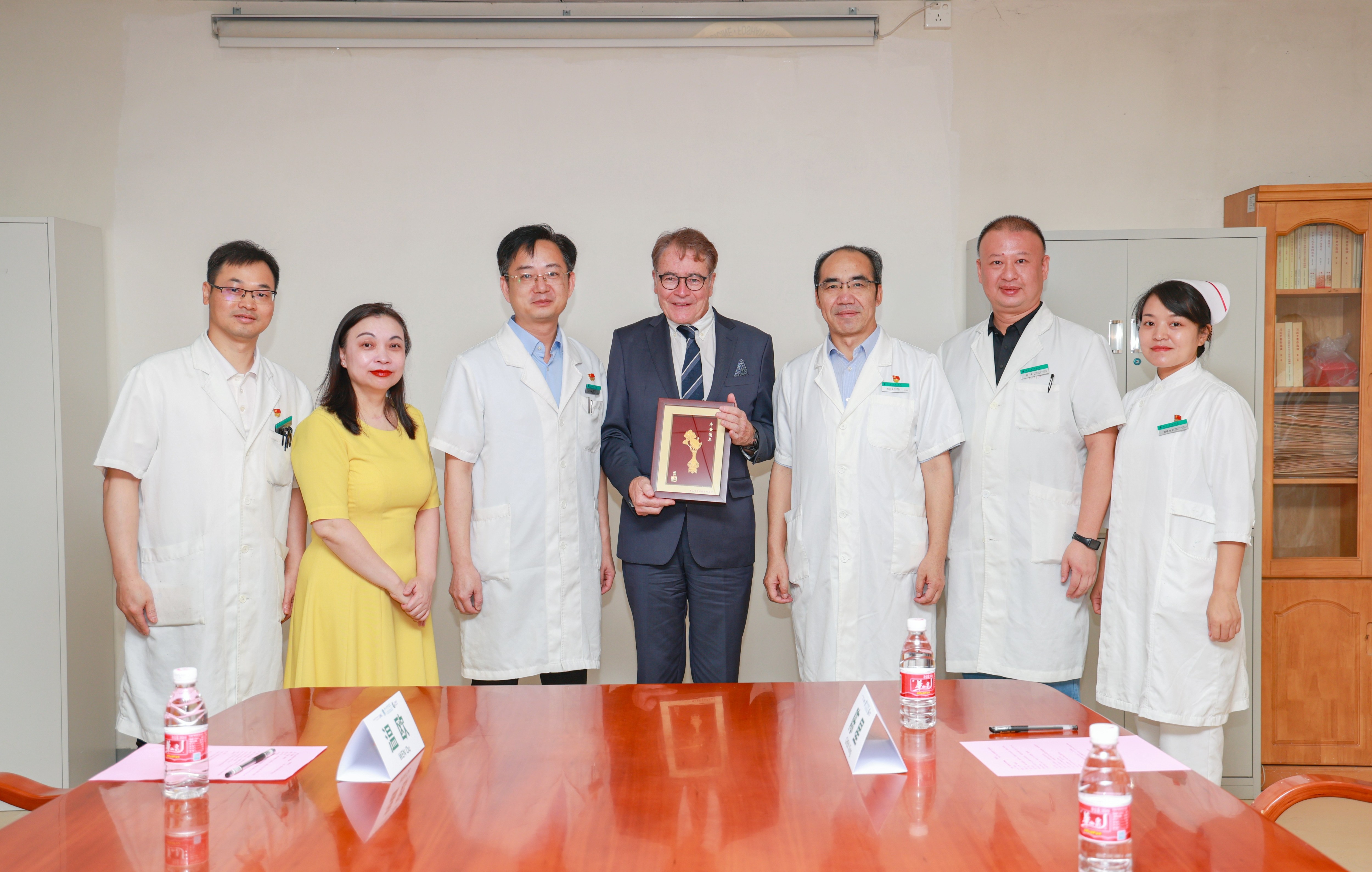
Welcome Ceremony
On the morning of June 16, Prof. ZHU Yongzhan, Director of the Foot and Ankle Department at Foshan Hospital of TCM, along with his team, held a welcome ceremony for Dr. Stinus. The event commenced with welcoming addresses by JIANG Kaiping, Secretary of the Party Committee of the hospital and Prof. ZHU Yongzhan. Dr. Stinus delivered an opening speech, followed by detailed introductions of the respective hospitals.

Doctor BAI Wenbo introduced the Foot and Ankle Surgery Department (Foot and Ankle Center) of Foshan Hospital of TCM. Established in May 2015, it is among the first specialized foot and ankle centers in China. The department integrates traditional Chinese medicine treatment concepts with modern medical technologies, focusing on the diagnosis and treatment of limb fractures and deformities, osteomyelitis, foot and ankle trauma (including bone, tendon, ligament, cartilage, and soft tissue injuries), sports injuries (such as Achilles tendon rupture reconstruction, minimally invasive repair of anterior talofibular ligament, and ankle impingement syndrome), as well as foot and ankle deformities including hallux valgus, flatfoot, cavus foot, and diabetic foot.

Subsequently, Dr. Stinus introduced himself and provided a detailed overview of his private clinic, Stinus Orthopädie GmbH, the University Medical Center Göttingen, and its Department of Trauma, Orthopedics and Plastic Surgery. He stated that his private clinic is located in Bovenden, Göttingen,, primarily treating patients with foot and ankle joint deformities, degenerative diseases, and spontaneous osteonecrosis of the knee (SPONK), with an average monthly outpatient volume of 40 to 50 patients. As the fourth-generation successor of Stinus Orthopädie GmbH, he expressed his pleasure in sharing that this year marks the company’s 120th anniversary, with a celebratory event scheduled for July 25. After more than a century of development, the company now operates 12 branches across eight locations in southwestern Germany, employing 91 staff members and specializing in orthotic device fabrication, orthopedic corrections, and rehabilitation technologies.

As a senior consultant of foot and ankle surgery at the University Medical Center Göttingen, Dr. Stinus emphasized the hospital’s integration of medical care, research, and teaching. The Department of Trauma, Orthopedics and Plastic Surgery is a premier trauma center in Germany, annually treating over 800 polytrauma patients and approximately 300 cases of severe trauma. Under the leadership of Prof. Lehmann, the department maintains a scientifically structured organization encompassing a regional trauma center, plastic surgery, pediatric orthopedics, advanced joint replacement center, and foot and ankle section.
Director ZHU Yongzhan expressed hope that Dr. Stinus’s visit would serve as an impetus for establishing closer and long-term collaborative relationships between Foshan Hospital of TCM and German colleagues.

Following the ceremony, ZOU Yunxuan, a chief physician of the Foot and Ankle Department, and the foot and ankle team, accompanied Dr. Stinus to visit the Traditional Chinese Orthopedic Splint Exhibition Wall, and observed nurses applying splints to immobilize joints. Doctor ZOU introduced these splints, which are made from fir wood and come in various sizes, designed to stabilize different joints. Compared with plaster casts, these splints offer superior breathability and allow X-ray imaging without removal.

Thereafter, Doctor ZOU accompanied Dr. Stinus to visit the Foshan sub-center of Shanghai Jiao Tong University Medical 3D Printing Innovation Research Center at the hospital. Doctor ZOU explained the applications of 3D-printed products and toured the 3D printing workshop. Doctor ZOU stated that the 3D-printed molds are mainly used for preoperative prosthesis adaptation to ensure surgical accuracy.

Special Lectures and Case Discussions
On the afternoon of June 16, Dr. Stinus presented a special gift to Director ZHU Yongzhan - a personally authored copy of his monograph Pedorthotics, signed with heartfelt wishes on the flyleaf. This precious gift embodies Dr. Stinus’s academic achievements and expresses his sincere hopes for enduring Sino-German friendship and future cooperation in the field of foot and ankle surgery.
Following this, Dr. Stinus delivered an internal lecture entitled Development and Medical Applications of Orthotic Footwear in the Foot and Ankle Department’s conference room. Beginning with the historical origins of footwear, he highlighted that shoes have evolved from mere aesthetic items to critical protective, supportive, and stabilizing devices for the foot, with widely recognized medical value. Regarding various foot deformities, he emphasized that orthotic insoles, shoe linings, and shoe structures should be individually customized to achieve effective treatment and rehabilitation outcomes.

After the lecture, an animated discussion ensued. Director ZHU Yongzhan remarked that the demand for orthotic footwear is continuously increasing with vast market potential. Although many orthotic insole products have emerged domestically, a more comprehensive customized orthotic shoe production chain remains to be developed.
During the subsequent case discussion session, Dr. Stinus and the foot and ankle team engaged in in-depth academic exchanges. The focus was a female patient in her sixties presenting with flatfoot, forefoot abduction, mild hindfoot valgus, and tenderness over the calcaneocuboid joint. The preliminary diagnosis was progressive collapsing foot deformity (PCFD) accompanied by calcaneocuboid arthritis. Imaging revealed talar tilt, collapse of the talonavicular and navicular-cuneiform joints, with severe and difficult-to-correct arch collapse. The team decided to perform flexor digitorum longus tendon transfer, spring ligament augmentation, medializing calcaneal osteotomy, and calcaneocuboid joint debridement. Regarding this case, Dr. Stinus shared his treatment strategy, recommending priority removal of calcaneocuboid osteophytes followed by talonavicular and calcaneocuboid joint fusion. Considering the patient’s mild flexible flatfoot and slight hindfoot valgus, he also suggested that arthroereisis could be considered to further improve the arch structure.
Case Discussions
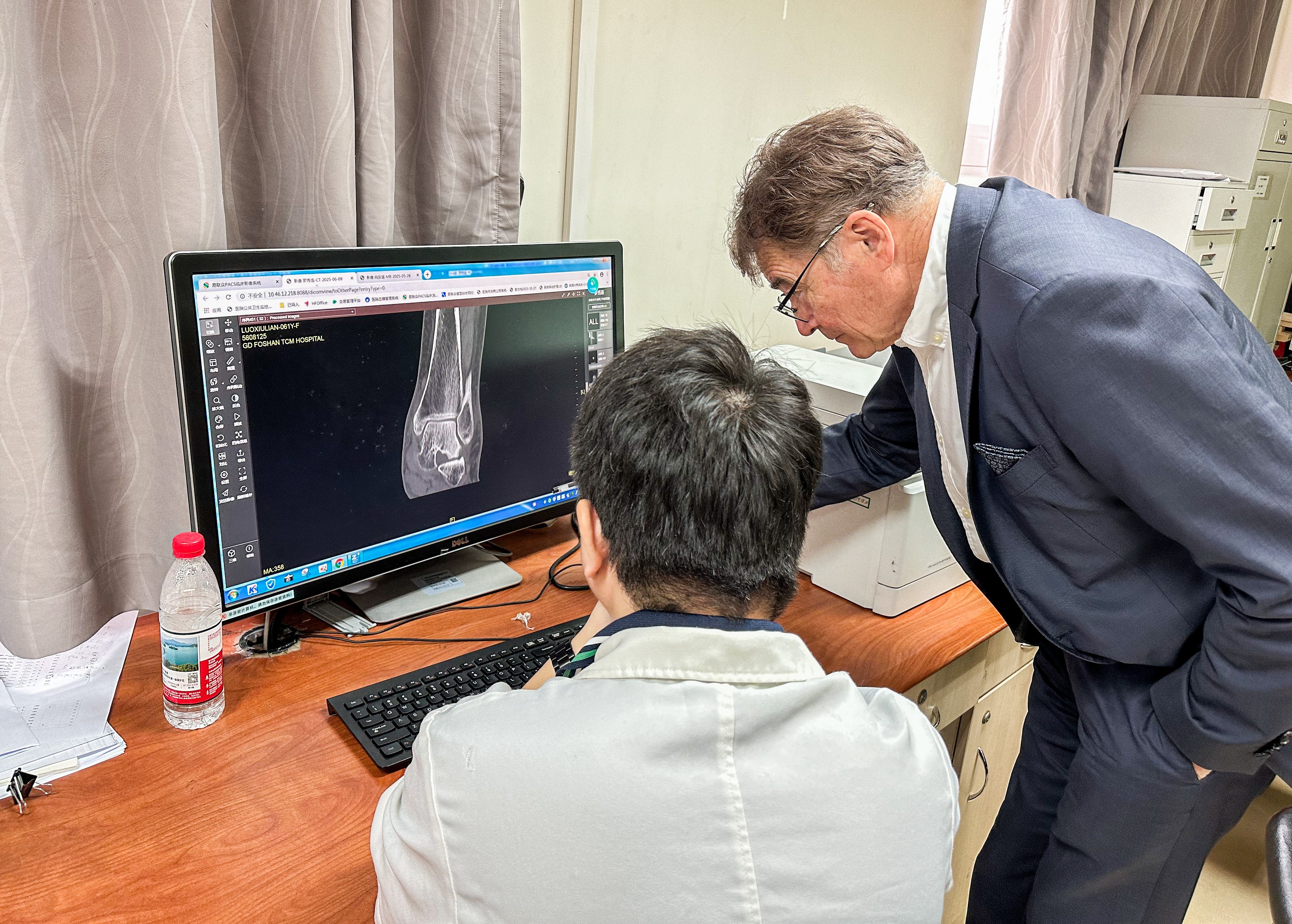
On the morning of June 17, Dr. Stinus and the foot and ankle team held a session in the conference room to discuss complex cases. Doctor LI Xue, an associate chief physician, presented a patient with talus fracture nonunion. Upon reviewing MRI images, Dr. Stinus identified signs of talocalcaneal joint fusion. After further evaluation of the fracture site and surrounding soft tissues, he proposed various surgical approaches. Dr. Stinus noted that the nonunion may be related to pathological fusion of the talocalcaneal joint and recommended surgical joint release along with reconstruction of subtalar joint stability to restore foot alignment and balance, thereby ensuring long-term functional recovery. He also shared experiences from similar cases and provided detailed guidance on accurately identifying concurrent lesions on imaging, emphasizing the importance of individualized treatment plans.

The second case involved a 61-year-old female patient with bilateral flatfoot deformity, with marked deformity on the left foot. Imaging revealed talocalcaneal joint fusion on the left side. Given the patient’s concomitant Parkinson’s disease, Dr. Stinus and Doctor LI agreed that foot stability was paramount. They recommended triple arthrodesis (fusion of the subtalar, talonavicular, and calcaneocuboid joints) to effectively correct the deformity, alleviate pain, and reduce postoperative complication risks related to the underlying disease.
The third case concerned a 14-year-old male patient who had sustained a sharp penetrating injury to the left foot, initially treated as a superficial wound. Two to four months post-injury, ultrasound examination revealed complete rupture of the posterior tibial tendon. The team performed tendon debridement and transfer of a plantar tendon. Dr. Stinus approved this management approach and suggested that flexor digitorum longus tendon transfer could be considered as an alternative. He noted mild elevation of the first metatarsal column with slight forefoot supination. Given the absence of significant structural foot deformity and only a history of trauma, he recommended conservative treatment with dynamic monitoring of functional recovery, advising against surgical intervention at this time.
Lastly, Dr. Stinus and Doctor YANG, an associate chief physician, had an in-depth discussion on the treatment of Mueller-Weiss disease, which is relatively prevalent in Guangdong province. Patients commonly present with chronic midfoot pain. Dr. Stinus noted that the etiology of Mueller-Weiss disease remains unclear, and the primary therapeutic goal is pain relief and functional improvement. Conservative treatments such as extracorporeal shockwave therapy and orthotic footwear incorporating lateral heel wedges can effectively alleviate symptoms. Surgical intervention, including joint fusion or lateral calcaneal osteotomy, may be considered when conservative measures fail or symptoms significantly worsen, aiming to restore foot alignment and improve quality of life.
Outpatient Activities
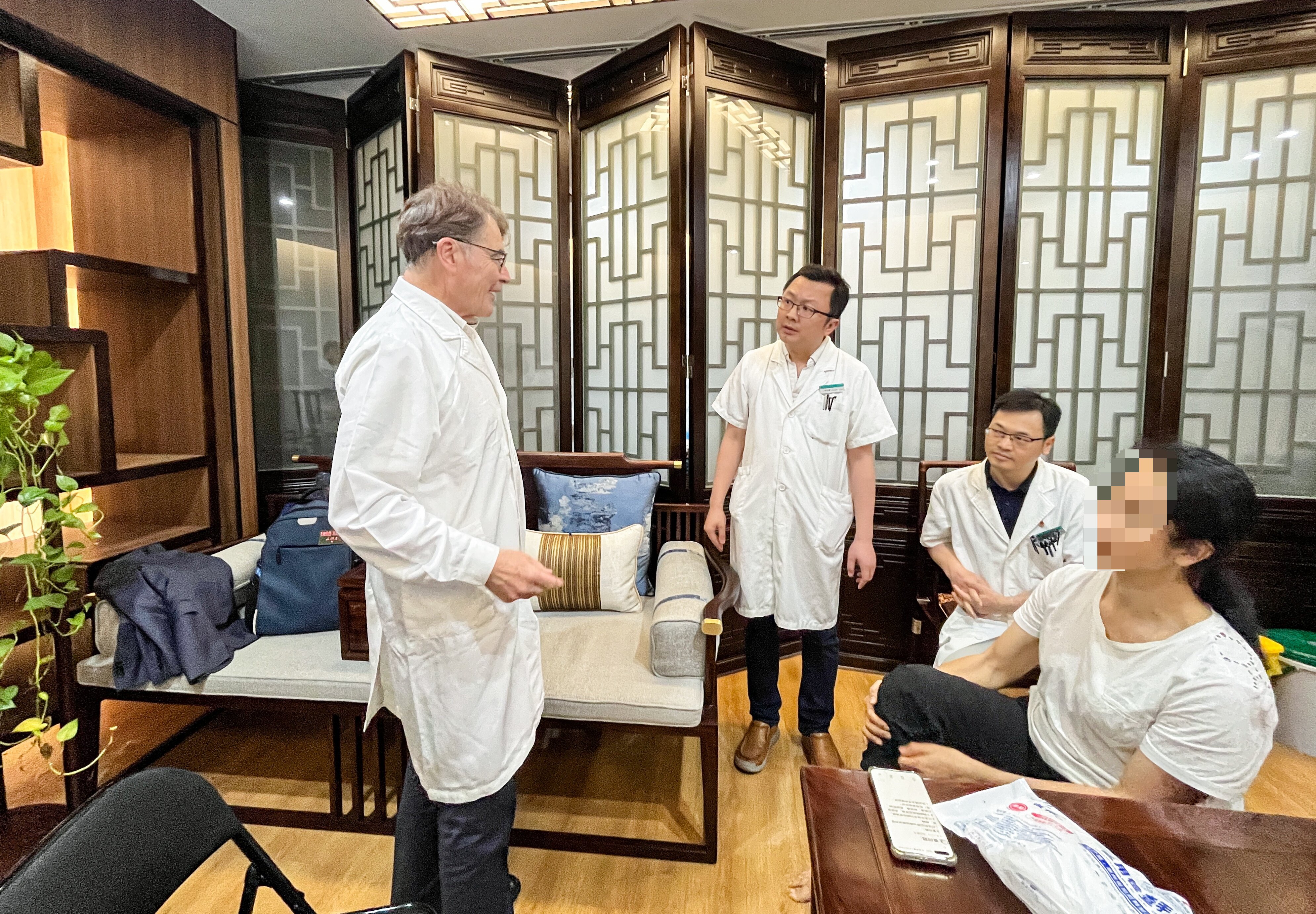
On the afternoon of June 17, Dr. Stinus, together with SHEN Guodong, Deputy Director, ZOU Yunxuan, a chief physician, and other doctors from the Foot and Ankle Department, attended the foot and ankle outpatient clinic. They saw six patients and conducted rigorous and meticulous analyses and treatments for various complex foot and ankle conditions. During consultations, Dr. Stinus engaged warmly with patients, proactively greeting them in simple Chinese, which significantly alleviated patients’ anxiety. He also provided patients and their families with scientifically sound and reasonable diagnostic and therapeutic advice.

For a patient with a history of ankle sprain and prior hallux valgus correction surgery, Dr. Stinus emphasized the importance of addressing pain-related fear to facilitate active participation in rehabilitation. He recommended incorporating exercises such as single-leg balance and gait training to restore function. Additionally, he advised the use of athletic footwear with a rocker sole and a 2 mm lateral wedge to optimize plantar pressure distribution, thereby alleviating excessive load and discomfort on the second and third metatarsals as well as the lateral midfoot.
Regarding a young female patient with a left ankle sprain and complaints of ankle pain, Dr. Stinus detected mild ankle instability through palpation and suspected ligament injury. He advised further diagnostic evaluation via ultrasound or dynamic fluoroscopy to clarify the diagnosis.
When assessing a 13-year-old female patient with congenital clubfoot, Dr. Stinus noted severe restriction of ankle joint motion, with almost no dorsiflexion, plantarflexion, pronation, or supination, preliminarily diagnosing common peroneal nerve dysfunction. He recommended that the patient first undergo consultation with neurology to rule out neurological causes before proceeding with targeted treatment. A surgical plan involving medial calcaneal osteotomy was considered; however, X-rays revealed distal tibial deformity and external rotation of the knee, complicating the surgery. Ultimately, the team recommended staged surgery, with the first stage correcting the clubfoot deformity, followed by distal tibial wedge osteotomy in the second stage.

Dr. Stinus also evaluated a young male patient with a strong interest in basketball who presented with lateral right ankle pain. A preliminary diagnosis of ankle impingement syndrome was made, with palpation revealing localized tenderness inferior to the lateral malleolus. Dr. Stinus recommended initiating conservative management, including local corticosteroid injection or analgesic therapy. Should the pain recur, arthroscopic evaluation was advised to investigate potential intra-articular loose bodies or ligamentous injury. He also suggested screening for gout as a possible underlying cause of the ankle symptoms.

A 30-year-old female patient who had been bedridden long-term due to a lumbar compression fracture presented with bilateral foot weakness at night and transient inability to stand. After examination, Dr. Stinus confirmed normal ankle joint mobility and foot stability and recommended prompt neurological evaluation to investigate possible spinal-related neuropathies.
Lastly, Dr. Stinus attended to a male patient who had sustained multiple fractures in a severe traffic accident and was experiencing nonunion and poor healing following foot and ankle surgery. The patient reported numbness in the affected foot and a pronounced pulling sensation in the hindfoot, which worsened when walking. Upon palpation, Dr. Stinus found that joint mobility was preserved and considered two possibilities: symptoms induced by psychological factors or infection/inflammation in the heel region. He advised an MRI re-examination to clarify the cause and guide targeted treatment.

Throughout the outpatient clinic, many patients and their families observed attentively, creating a lively atmosphere. Dr. Stinus maintained a consistently warm and patient demeanor, conducting thorough physical examinations and providing detailed explanations. Before each examination, he courteously asked, “May I touch your foot?” and used simple Chinese phrases such as “Hello” and “Thank you” to establish good rapport. His affability and professional competence earned unanimous praise from all patients and their families.
Surgical Guidance
On the morning of June 18, Doctor LI Xue, an associate chief physician from the Foot and Ankle Department guided Dr. Stinus on a tour of the OR. Doctor LI explained that four operating rooms are routinely used for foot and ankle procedures, all of which are equipped with advanced fluoroscopy systems to enable real-time intraoperative X-ray guidance.

Subsequently, a triple arthrodesis procedure was successfully performed by the team comprising Prof. ZHU Yongzhan, Dr. Stinus, Dr. LI and other doctors.
During the surgery, Dr. Stinus demonstrated in detail the standard surgical approaches, joint surface preparation, osteophyte removal, and microfracture techniques. He then assisted Director ZHU in temporarily fixing the joint using Kirschner wires and adjusted the foot to achieve normal anatomical alignment.
During intraoperative fluoroscopy, Director ZHU and Dr. Stinus jointly evaluated the X-ray images, with particular focus on confirming the Meary’s line, calcaneal position, and the alignment of the subtalar and talonavicular joints to ensure a satisfactory corrective outcome.
Special Lecture and Discussion Session
On the afternoon of June 18, Dr. Stinus delivered a specialized lecture titled Medical Principles and Clinical Applications of Orthotic Footwear in the Foot and Ankle Department conference room. During the lecture, Dr. Stinus systematically explained the classification of orthotic footwear, selection of raw materials, and structural design, emphasizing that the hardness and softness of the materials directly influence the support provided to the foot arch. He highlighted that a single structural design cannot meet the diverse needs of all patients with various foot conditions; therefore, customization and functional design have become the development trend. Dr. Stinus introduced the use of 3D foot scanning and plantar pressure thermography technologies to accurately capture foot data, thereby aiding the fabrication of personalized orthotic footwear. Dr. Stinus pointed out that for conditions such as flatfoot, high-arched foot, calcaneal varus/valgus deformities, metatarsalgia, and Morton’s neuroma, orthotic footwear combined with physical therapy, gait training, and spinal manual therapy (Chiropraktik) can effectively alleviate symptoms. Furthermore, orthotic devices play an important role during the rehabilitation phase after hallux valgus correction, joint fixation, and arthrodesis procedures.

Following the lecture, there was enthusiastic interaction. A doctor shared the use of a full-contact plaster cast utilized in foot and ankle practice, which requires long-term wear and cannot be removed by the patient, effectively improving patient compliance. Dr. Stinus expressed strong approval and emphasized the critical role of patient cooperation in treatment.

During the session, Dr. Stinus focused on the application of spinal manual therapy (Chiropraktik) to the foot and ankle joints. He provided live guidance to doctors: A doctor seated with knees slightly flexed and ankles in neutral position, Dr. Stinus applied sustained traction to mobilize the subtalar joint, supplemented by rhythmic oscillations and plantar soft tissue release, specifically targeting the plantar fascia and intrinsic foot muscles. The doctor who experienced the technique reported significant foot relaxation and improved joint mobility. Medical staff actively participated in the discussion, creating a lively atmosphere.

Finally, Doctor. LAI, an associate chief physician shared a case involving an 11-year-old child with bilateral flatfoot presenting with foot pain for over a year, predominantly on the right side, with poor response to conservative treatment. Physical examination revealed bilateral semi-rigid flatfoot with forefoot abduction, significant hindfoot valgus, and Achilles tendon contracture. Dr. Stinus recommended enhancing soft tissue release, Achilles tendon stretching, and gait training. If conservative management proved insufficient, surgical intervention could be considered. Both sides agreed that this case provided valuable clinical insights into pediatric flatfoot diagnosis and management.
Case Discussion and Surgical Guidance
On the morning of June 19, Dr. Stinus and the foot and ankle team focused on treatment strategies for foot fractures in polytrauma patients. Dr. Stinus emphasized that the primary treatment principle for such complex cases is to control soft tissue swelling and closely monitor local skin and vascular status. Regardless of the presence of multiple systemic injuries, early surgical intervention should be avoided, and treatment deferred until swelling subsides and soft tissue conditions permit. For acute foot fractures, Dr. Stinus and the team generally prefer temporary fixation using braces or external fixators, rather than immediate arthrodesis, to minimize secondary soft tissue damage.

Dr. Stinus particularly stressed that for complex foot fractures such as Lisfranc injuries and calcaneal fractures, locked plates (guiding plates) should be the first choice to achieve anatomical reduction and stable fixation, balancing early functional recovery with later soft tissue repair. Joint fusion should be avoided initially to preserve biomechanical function. After the patient’s overall condition and local soft tissue status stabilize, staged corrective or arthrodesis procedures may be considered based on subsequent recovery.
Later that morning, Dr. Stinus collaborated with SHEN Guodong, Deputy Director of the Foot and Ankle Department, to perform internal fixation surgery for a post-traumatic foot fracture sequela. Through close collaboration with Dr. Stinus, the surgical team attained precise fracture reduction and stable fixation using locking plates, with a strong focus on reestablishing the foot’s biomechanical axis to support postoperative weight-bearing. The procedure exemplified the principles of minimally invasive surgery and precise biomechanical control in foot and ankle reconstruction.

This case sharing and surgical demonstration fully reflected the high degree of professional consensus and consistency between Chinese and German foot and ankle surgeons in managing complex trauma-related foot injuries.
Special Lecture and Outpatient Activities
On the afternoon of June 19, Dr. Stinus delivered a specialized lecture titled Ankle Sprains: Conservative Treatment and Surgical Intervention in the Foot and Ankle Department conference room. The lecture commenced with an overview of the epidemiology of ankle sprains, followed by a systematic explanation of the classification of ankle sprains, treatment strategies for acute and chronic ankle instability, ligament injuries, and cartilage defects. Dr. Stinus emphasized that for isolated single-ligament injuries with good ligament end approximation on imaging, favorable clinical outcomes can be achieved with conservative treatment even in professional athletes. For patients with Grade II ligament injuries or pre-existing chronic ankle instability, anatomical reconstruction surgeries such as the Broström procedure significantly enhance joint stability. He underscored that surgical treatment can be effective not only during the acute phase but also when performed in a delayed manner after the injury. In cases of ligament deficiency, Dr. Stinus recommended reconstructive techniques including periosteal flap repair or gracilis tendon grafting, which can be performed via open surgery or arthroscopically. Notably, lateral ligament injuries of the ankle often present with a high rate of concomitant injuries, especially in athletes; thus, heightened diagnostic vigilance and comprehensive imaging evaluation are essential to avoid missed diagnoses. Additionally, Dr. Stinus highlighted that persistent syndesmotic instability in either the transverse or sagittal plane commonly results in prolonged recovery and suboptimal outcomes. Increasing evidence from evidence-based medicine supports early surgical intervention for any form of syndesmotic instability. The lecture was rich in content, effectively bridging theory and clinical practice, and provided valuable guidance to the attending physicians.


Following the lecture, a female patient suffering from Complex Regional Pain Syndrome (CRPS) sought consultation after learning of Dr. Stinus’s short-term visiting professorship at Foshan Hospital of TCM. Dr. Stinus first observed the patient’s barefoot gait and pivoting in place. The patient exhibited marked pain upon left foot ground contact, with pain intensifying during walking, accompanied by an obvious limp.
A thorough palpation examination of the patient’s left foot followed. No abnormalities were found in the forefoot region, and joint mobility above the Lisfranc line was normal, with no significant tenderness during palpation. However, in the hindfoot area, Dr. Stinus identified pronounced tenderness and Achilles tendon weakness, raising suspicion of partial tearing or chronic injury; calf muscle function was also impaired. For differential diagnosis, Dr. Stinus inquired whether the patient had undergone vascular Doppler ultrasound and recommended further interdisciplinary consultations with neurology, psychiatry, and pain management specialists to exclude vascular, neurological, or psychological contributors to the pain.
Regarding treatment recommendations, Dr. Stinus firmly advocated a “pain control first, surgery later” approach. He advised prioritizing systematic conservative therapies, including manual therapy, orthotic shoe use, acupuncture, and traditional Chinese medicine, supplemented by oral analgesics if necessary. Dr. Stinus cautioned that pain relief may require a 3 to 6-month period and warned that premature surgical intervention before adequate pain resolution risks pain generalization, potentially spreading discomfort throughout the foot and exacerbating the patient’s suffering.
On surgical timing, Dr. Stinus recommended that surgery be considered only when the patient can bear weight on the heel and perform dorsiflexion (toe-up walking) with no or minimal pain sustained over a period without recurrence. Only then should further discussion with a foot and ankle surgeon regarding operative options take place.
For pharmacological management, Dr. Stinus suggested stage-specific use of analgesics such as Novaminsulfon (marketed as Novalgin in Germany), topical morphine patches (Tilliclin), and conventional nonsteroidal anti-inflammatory drugs (NSAIDs) like ibuprofen.
Special Lecture
On the morning of June 20, Dr. Stinus delivered a specialized lecture titled Hallux Valgus: My Strategies in the Foot and Ankle Department conference room. He systematically explained the diagnostic criteria, treatment strategies, types of surgical procedures, and key points of postoperative rehabilitation for hallux valgus. Dr. Stinus first emphasized that the diagnosis of hallux valgus should be based on a combination of clinical presentation and imaging evaluation. X-rays are essential, with measurements such as the hallux valgus angle (HVA) between the first metatarsal and the proximal phalanx, and the intermetatarsal angle (IMA) between the first and second metatarsals, used to assess the severity of the deformity. For mild deformities or asymptomatic patients, conservative treatment including orthotic shoes, gait adjustment, and physical therapy can be effective.
When the deformity is more severe or symptoms are pronounced, surgical options should be chosen based on individual patient factors. Dr. Stinus highlighted commonly used osteotomies, including Chevron, Scarf, and Akin osteotomies, providing detailed explanations of their indications, surgical steps, and precautions. During surgery, lateral joint capsule release is typically performed to correct the valgus deformity. Dr. Stinus pointed out that while the Scarf osteotomy provides good correction, postoperative complications such as “troughing” - medial collapse due to sliding at the osteotomy site - may occur. Research indicates that combining Scarf with Akin osteotomy achieves better correction results in moderate to severe hallux valgus patients.
Regarding postoperative management, Dr. Stinus stressed the importance of functional rehabilitation, including early weight-bearing, use of foot orthoses, and training of hallux mobility, which help reduce complications and improve long-term function.
Additionally, Dr. Stinus provided a thorough introduction to the indications, contraindications, and surgical techniques of the Lapidus fusion procedure. This technique is suitable for patients with instability of the first tarsometatarsal joint, severe hallux valgus, or associated internal rotation deformity of the first metatarsal. The Lapidus fusion effectively corrects severe deformities and controls forefoot load distribution, but carries a risk of joint stiffness, necessitating strict adherence to indications. Dr. Stinus also detailed fixation methods, postoperative weight-bearing protocols, and rehabilitation exercises following Lapidus fusion.
The lecture was comprehensive and focused on key surgical points, offering an in-depth analysis of systematic treatment strategies for hallux valgus. Attending medical staff benefited greatly from the session.
Closing Ceremony
On the afternoon of June 20, the closing ceremony for Dr. Stinus’s visiting professorship were held in the Foot and Ankle Department conference room. Prof. ZHU Yongzhan, Director of the Foot and Ankle Department, attended with his team.

In his speech, Director ZHU expressed sincere gratitude for Dr. Stinus’s visit. He noted that although the exchange period was brief, Dr. Stinus brought inspiring academic presentations and precise, meticulous surgical guidance, which greatly contributed to expanding the team’s clinical thinking and academic horizons. This visit further strengthened the excellent foundation for Sino-German collaboration in foot and ankle surgery and provided opportunities for ongoing cooperation.
In his reply, Dr. Stinus expressed his honor in being invited to Foshan Hospital of TCM to engage in academic exchange and clinical discussion with esteemed colleagues. During the five-day exchange, he deeply appreciated the team’s rigorous clinical approach, surgical skills, and professional spirit. He especially thanked the team for their careful arrangements and expressed openness and anticipation for further collaboration in the field of foot and ankle surgery.
As an academic memento of this visit, Dr. Stinus presented the team with two authored monographs, to support their continued learning and reference.


The closing ceremony concluded smoothly in a friendly and pragmatic atmosphere, with group photos marking the successful conclusion of the visiting professorship event.
