-
News & Events

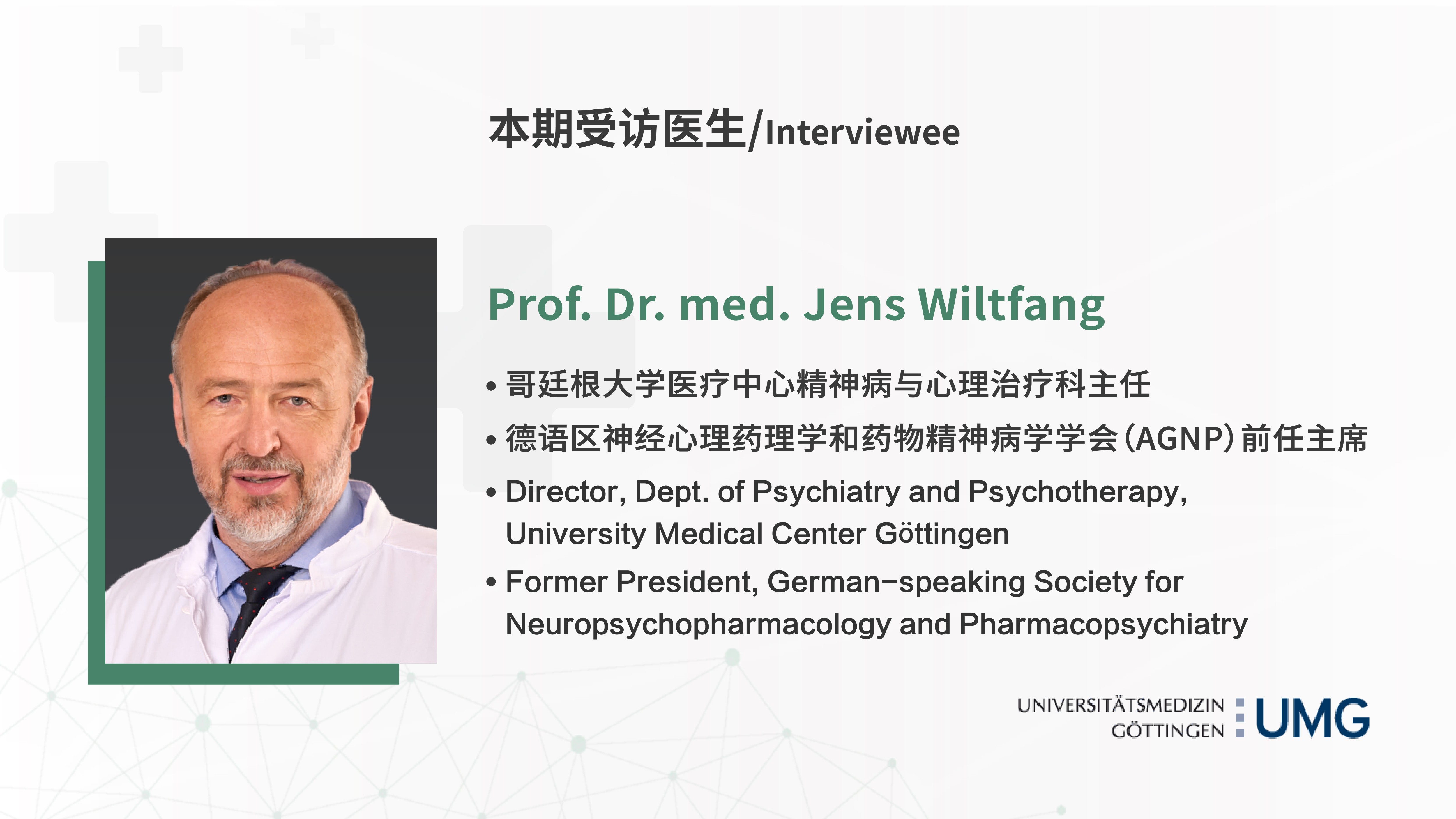
For EPISODE 17 of the World’s Great Doctors, it is our great honor to have Prof. Jens Wiltfang as our distinguished guest, who is the Director and Chairman for Psychiatry and Psychotherapy at the prestigious University Medical Center of Göttingen and former President of the German-speaking Society for Neuropsychopharmacology and Pharmacopsychiatry(AGNP).
Back in 1980s, Prof. Wiltfang developed a polyacrylamide gel system called SDS-PAGE when he was a young researcher. And few years ago, after decades devoted in research, Prof. Wiltfang developed a system called Aβ-2step-Immunoassay together with his team. Prof. Wiltfang’s team is among the groups who develop biomarker-guided early diagnostics of Alzheimer's dementia. By cost-efficient blood assays, they are now able to diagnose Alzheimer's dementia fifteen years before it precipitates as dementia. Years ago, Prof. Wiltfang would have been part of the team led by a Nobel Prize winner, but he never regrets that he took the decision of going back to clinical medicine because his vision was to contribute to the early diagnosis of Alzheimer’s disease with biomarkers. During the interview, Prof. Wiltfang also updates us with the development of several monoclonal antibodies in treating Alzheimer’s disease.
1. Why did you decide to pursue a career in medicine and why, in particular, did you decide to specialize in Alzheimer’s Disease?
Yes, actually, it was a process of excluding things which I didn't want to do. My father was a really well-known lawyer and so I thought maybe studying law would be an option. But for me, it was a little bit too boring and not interesting enough. And then I thought medicine could be much more interesting because of all the physiology and that you can be of some support for people. So finally I decided to study medicine. In Germany, you had to have an excellent school exam, otherwise, you wouldn't have a chance to get a place at the university. This is still the case that maybe only 15-20% of the best students are allowed to apply for medical studies. I was lucky that I had a good school exam, so I could apply for medicine and chose Medizinische Hochschule Hannover (MHH), which is close to Göttingen because I come from the northern part of Germany. My brother was studying in Göttingen. He is one of the most famous dental and jaw surgeons now in Germany and he has a Chair of dental and jaw surgery in Kiel, the northern part of Germany. We were both studying medicine, my brother in Göttingen and me in Hannover.

Prof. Wiltfang's brother Prof. Dr. med. Jörg Wiltfang
Why did you decide to specialize in Alzheimer's disease?
This was actually due to the fact that after my studies of medicine in Hannover, I got a scholarship from the Max Planck Society in Germany which offered me a stipendium from the German Research Foundation (DFG). This allowed me to enter, for three and a half years, basic science at the Max Planck Institute of for Experimental Medicine in Göttingen. Directly following my studies, I did three and a half years of basic research, mostly dedicated to protein biochemistry. I learned, in those years, a lot of basic technologies of protein biochemistry, cell biology, etc. This actually was the basis to specialize in Alzheimer's disease because it became obvious that you need more and more biomarkers for an early diagnosis of Alzheimer's dementia and of preclinical Alzheimer's dementia. I got all the tools and all the know-how - mass spectrometry, immunoprecipitation working with antibodies, etc in the years within the Max Planck Institute. When I then joined the University of Göttingen to do my specialization in Neurology and in Psychiatry, I did both specialties and was certified as a neurologist and psychiatrist. During this training, the former director of the department allowed me to have formed the sketch of my own lab and my own group. This is the reason why I specialize in Alzheimer's disease actually - because I had all the tools, and, during this time I developed a completely new system, a gel system, polyacrylamide gel system, which is called SDS-PAGE, which allowed us to separate, for the first time worldwide, the so-called Aβ peptides, which implicated in the pathophysiology of Alzheimer's dementia. In those days, this was 1986, it was not possible to separate those Abeta-peptides Aβ peptides and at the same time detect them in the lower picogram amount by western blotting, and this was then possible by this new method which I developed together with Dr. Hans Klafki, who is now part again of my team. He went then to the big Pharma Novartis, Schering, and Bayer but then ultimately came back into my team. This gel system, this urea SDS-PAGE gels are worldwide used in basic research in Alzheimer's dementia all around the world, but they were invented during my time at Max Planck Institute. This was another reason why I entered this field.
I think we will touch this again later, but I can already make the point that it is important that if you want to enter a university career or a research career in medicine, you bring in new methods and new methodology. You do some, maybe two to three years, training in basic science or studying in parallel informatics, maybe to use artificial intelligence. So it is important to offer something outstanding and some interdisciplinary work with guys coming from chemistry, from physics, to shed new light on medicine because this will allow you to solve and tackle questions that others are not successful to solve because all other guys are also smart. You have thousands of students in China, and thousands in the U.S., in average we have the same intelligence as the average. What makes the difference is that you bring in new methods and new thoughts. This makes a difference.
2. Who have been the most influential people throughout your career? What did they teach you, and how did they inspire you?
I would say, first of all, my parents. My mother was a teacher and the director of a school, and my father was a lawyer who had high analytical intelligence and was really good at mathematics. Both parents did a lot of reading and were really interested in life sciences, not being in life sciences but nonetheless, they were very interested in life science. This was the first stimulation.
Then the supervisor of my doctorate thesis was very important to me. His name was Prof. CKanzler at the Medical School of Hannover (MHH). Unfortunately, he is not among us anymore anymore.
Then Prof. Neuhoff at the Max Planck Institute forof Experimental Medicine, Göttingen, head of the Department of Neurochemistry, actually wanted that I should stay in basic science. I was offered a scholarship at the Rockefeller University New York at the lab of Paul Greengard, who won, several years later, the Nobel Prize. So I would have been part of the team when he did win the Nobel Prize. But I decided to go back into medicine and I never regret that I took this decision because I just wanted to have the methodology in protein biochemistry to make use of very low abundant what was sensitive biomarkers in the human body fluids bloods to diagnose diseases. etc, so I didn't regret this. But he was really stimulating my career …… when I came to ask him when I have to start and when we usually have to leave. hHe said: "I don't care if you come at 5 pm and work all night. I don't care at all. You only have to be successful. That's the only thing." This is not the case anymore now but in 1986 there was a lot of money, the Max Planck Society was very rich, so I could order all the equipment I needed for my research. The work atmosphere was really free. There were no really fixed working times. It was really free science. This is not the case anymore now. But in those times, it was the case. So he stimulated me very much in my research.
Then in the clinics, when I entered the training of neurology and psychiatry, it was Prof. Rüther, the hHead of the Department of Psychiatry, who is still living now in Munich. And Prof. Felgenhauer who was the hHead of the Department of Neurology. Both of them really supported my career and both are the most important ones.
3. As a professor, a physician, a clinic kinik director, a scientist, how do you balance your personal life, administration, clinical practice, research activities and lecturing?
Yeah, so first of all, you need a wife which is a little bit crazy like you. My wife is also a medical doctor, and she's working in nuclear medicine, so she knows what a life of a university professor and director in medicine means - you have to be very flexible … that there may be a meeting on the weekend and you have to fly to Barcelona or whatever. This is only possible if you have a relationship with a the partner, in this case, my wife, who knows what I talk about because she comes from medicine too.
And then you have to have an excellent team. Over the years, I was really lucky to hire a really outstanding team of senior residents, so I can delegate some of my duties. I see my own patients, I have my ward rounds, I do my lectures, but unless you have an excellent team of people, you cannot be so successful to run a large university clinic with seven chairs associated to my clinic, including my own chair and six other chairs. We have twenty research groups and six chairs. We do a lot of research covering a wide span from imaging research, functional MRI, psychotherapy research, but also really in-depth protein biochemistry, animal models, synaptic plasticity, optogenetics etc,.
Two of the chairs are bridging chairs, one with the Max Planck Society, so I have all the equipment of the Max Planck Institute for protein biochemistry because Olaf Jahn is the chair of this professorship. He is at the same time responsible for the protein biochemistry service of Max Planck. And the other chair is with the Helmholtz Gesellschaft, this is held by André Fischer, he is at the same time the Director of the German Centre for Neurodegenerative Diseases, site Göttingen. He is a worldwide well-known expert for epigenetics. This allows me to have all the facilities of micro-RNA Micro-MRI screening and epigenetics.
And then I have two chairs that are cross-bridging with the U.S., one is held by Torsten Klengel, he's working halftime in Harvard in the U.S. and halftime in Göttingen. The other is held by Dr. Olaf Schlüter who works halftime in Pittsburgh and halftime in Göttingen. He's an expert in optogenetics and diseases of the synapse and in the pathophysiology of the synapse which is really important for Schizophrenia, the development of addiction dependencies, and other diseases related to a lot of issues where you have problemsto in synaptic dysfunctionplasticity.
So we cover a wide range of research, from psychotherapy research to really specific molecular psychiatry. Some of our these students are really surprised when they enter psychiatry for the first time. They have a completely different image of psychiatry - all these crazy people, all these psychiatrists who only talk and they have just their rating scales, and that's it. But modern psychiatry is completely different.
So there's a strong move in psychiatry and it’s steadily progressing. Modern psychiatry has this move which neurology experienced, let's say, in the seventies, with mMagnetic resonance imaging (MRI) coming up. Psychiatry has gained a completely different speed of development due to epigenetics, positron emission tomography coupled with MRI technology, the hybrid imaging. And there's a lot of ongoing research in biological psychiatry, and molecular psychiatry. And then the students reactare like: wow, I didn’t know this before! This motivates And then a lot of students want to join the department.
4. You enjoy a great international reputation. What is your proudest career achievement to date and why?
Yes I think actually as I said we are well known in the field of biomarker-guided early diagnostics. So I already told you that as a young researcher I developed this gel system which is in use worldwide in basic science in Alzheimer's research. And we are together with some other groups like Bateman´s group in US or Kaj Blennow and Eric Zetterberg in Sweden and a group in Japan, which is headed by the Nobel prize winner for mass spectrometry. We are among the groups who develop biomarker-guided early diagnostics of Alzheimer's dementia and we are now able to diagnose Alzheimer's dementia already fifteen years before it precipitates, actually, as dementia, by blood assays. Before it was only possible by cerebrospinal fluid assays, but this doesn't offer you such a widespread diagnostics screening because it's not minimally invasive and it's a bit painful. But blood is easy accessible and can be used during follow-up to monitor the disease progression and the treatment efficacy.
Another brand new system that we developed, we call Aβ-2step-Immunoassay. We developed this very recently, and this method is based on e a first immunoprecipitation (IP) from blood by a fully robotic system where we use magnetic micro particles coated with antibodies, then we extract the Aβ peptides from blood by this pipetting robotics, next we developed a new method to elute the concentrated and purified Aβ peptides from the magnetic particles, and this elution procedure directly allows that the eluate can go on commercially available ELISA platforms like the Elecsys™ exis system of Roche Diagnostics or other systems like the Lumipulse™ system of Fujirebio, whatsoever. And this, allows us, together with some phospho-Tau epitopes to diagnose preclinical Alzheimer's dementia fifteen years before it really becomes clinically overt and manifest. This now allows us to systematically investigate, secondary preventive interventions , because if you can identify such patients years before the dementia comes, then you can check what drug or maybe which non-pharmacological intervention can stop or, kind of, prevent the development of Alzheimer's dementia.
So, to summarize this, my proudest career achievements are: , as a young scientist, the development of this specific urea SDS-PAGE gel system and a few years ago, the development of the Aβ-2step-Immunoassay combining robotic immunoprecipitation with a fully automated antibody-based quantification of Aβ peptides in blood. So, the two methods I developed, one as a young student and one as a senior professor.
5. What’s the biggest challenge in the field of Alzheimer’s Disease? What’s the trend of AD in the coming decade?
The biggest challenge is the disease-modifying treatment. Disease-modifying means preventive treatment. And you may know that now there's a game changer, I think, coming, which are monoclonal antibodies which specifically can bind this soluble (Abeta) oligomers or specifically neurotoxic Abeta peptide species . One of those antibodies was approved by the FDA in the US but not in Europe because European colleagues were not completely convinced that this antibody may have a sufficient treatment efficacy, it's called Aducanumab. I think that it has a good chance to prove finally that it does have treatment efficiency, there's now a third-phase worldwide study ongoing to validate this. But there's another antibody called Lecanemab which has been approved by the FDA and I think this will be approved by the EMA in Europe this year. I guess will be available in Germany maybe in early 2024. This antibody also has demonstrated that it can slow down the speed of disease progression, so it is not a symptomatic treatment. What we have now arecholinesterase inhibitors and memantine but these are only symptomatic treatments and they don't slow down the disease progression - but those monoclonal antibodies do; and there's another one from Lilly, Donanemab, which will be unblinded, I would guess, April or May latest this year and the results will be presented at the AAIC congress (in Amsterdam, 2013). It is also promising. We will see. But the phase-IIIstudy, is not de-blinded. The phase-II studies were very promising. So now, for the first time in Alzheimer’s disease research, we have the first evidence that it may be possible really to have a disease-modifying and preventive therapy. Of course this is only the beginning, as part of a treatment combining different targets like drugs dedicated to slow down tau aggregation, but this is the start.
Like in multiple sclerosis therapy neurologists were really successful now to have more and more smart combination therapies. I think this will be the start to devise and identify the most important or the most successful combination therapies. But so far, all research and all clinical studies for decades were not successful in identifying any drug which is really preventive and really modifying disease progression. Now, for the first time, after decades of research, we have evidence by those monoclonals directed against Aβ peptides that it seems to be possible. So that's a really good news for all the millions of people affected worldwide and it is also very important for China because your society is overaged like our society.
And you know age is the highest risk factor for Alzheimer’s dementia, simply aging. The average life expectancy of a girl born today is extrapolated to be ninety years. And so far the predictions have been true. What has been predicted in the 1960s what the life expectancy should be in 2020 was validated. So I think this is correct that a girl born today, may have an average life expectancy of ninety years. But you have to know that all those people who become at least ninety years will become with 30% prevalence of dementia. So every third of being ninety years or older will develop dementia and one in two dementia are Alzheimer’s dementia. So you can say that every girl worldwide which is born today has a risk of 1.5 out of ten to develop Alzheimer’s dementia. This is the fact, this is known among experts. So it's very important to develop disease-modifying treatments.
Alzheimer's dementia wasn’t the problem, let's say in 1905, or 1910 when Alzheimer was living because average life expectancy was much lower. Dementia was not an issue because people died before. With the ageing of societies, now dementia becomes a significant problem. The peak incidence of Alzheimer's dementia is 78 years. Decades before, only a few people became 80 years or older, most died before.

Dr. Alois Alzheimer (1864-1915), known for the first published case of "presenile dementia" (Alzheimer's disease)
6. On January 31, Xuanwu Hospital in Beijing reported the world's first case of a 19-year-old adolescent with Alzheimer's Disease, which has recently become a hot topic among the general public. Is it true that AD is becoming more prevalent among the younger population? Should young people take some preventative measures?
Of course they should take preventive measures, and they should live a healthy life whatever. But the incidence or the prevalence of Alzheimer's dementia among the young is not increasing worldwide. This so-called type II Alzheimer's dementia is a dementia before the age of 65, especially if you're very young, let's say 40 or younger. The overwhelming majority is due to point mutations, the autosomal dominant inherited point mutations on the beta-amyloid precursor protein, on presenilin 1, that is most of the mutations, and some on presenilin 2. If you know that you have such a point mutation, you unfortunately will develop AD. There are more than 130 point mutations known, but they make only 1% of all the AD cases so roughly only 1% but not much more are really genetic-driven Alzheimer's disease cases. The rest are familial cases, but this only means that your mother, your father or grandfather developed Alzheimer's dementia so you have a kind of a load in the family, but there is no autosomal dominant inheritance, this just implies a little higher risk, this is called familial AD. But the genetic AD makes not more than 1% of the cases and only the genetic ADs has this really really young cases being affected, but the incidence and prevalence of those cases has been constant for decades and I don't think it will change.
7. In comparison to degeneration of other parts of the body, such as the joints or the spine, it is difficult to detect neurological degenerative diseases, such as Alzheimer's disease, in their early stages. How can caregivers of the elderly detect AD symptoms as early as possible? And how do you tell the difference between AD-caused cognitive impairment and normal aging-related memory lapses?
Actually it's also already expressed in your sentences that the first symptom of the dementia due to Alzheimer's disease is cognitive impairment in the area of memory, memory consolidation and retrieval of stored information.This is the first symptom of Alzheimer's dementia that you have problems in memorizing. If you only have problems in memorizing which can not be validated by common screening test and you think “oh I'm afraid something is coming up”, this is called subjective cognitive deficit(SCD). The next stage which is called prodromal Alzheimer's dementia is mild cognitive impairment (MCI). In mild cognitive impairment, you are also able to deal with daily life activities - you can still be able to drive your car and with writing little little notices, you can manage your day. You have not such a significant impairment of your everyday life routines that it can already be called dementia.You are only allowed to diagnose dementia, if core activities of daily living are impaired. This is not the case in mild cognitive impairment, but in contrast to subjective cognitive deficits, in mild cognitive impairment, the usual screening tests like DemTect , MoCA and so on give a pathological test result so you can diagnose (MCI). So the first stage is subjective cognitive deficit, if you had all your life a good memory, you and your friends may know something is ongoing, but the usual screening test don't yet give pathological test results. Then you have enter cognitive impairment, and then you develop dementia, with early dementia, moderate dementia, and severe dementia.
Now you have to know when it comes to the second part of your question that you may have mild cognitive impairment or subjective cognitive deficits, if you for example have depression in the elderly, which can be late onset depression -and due to depression, you have also neurotransmitter imbalance which affects cognition and you can have more or less the same memory deficits as in AD. You cannot differentiate this really precisely - you need biomarkers. The biomarkers available are Amyloid PET and biomarkers in cerebrospinal l fluid and most recently - we work in this field the blood biomarkers which will enter routine diagnostics, I would predict latest within two years. - then it will be available as part of routine diagnostics. For example, if this memory deficits are due to depression, or stress, prolonged stress, or whatever, then the biomarkers are not changed. Thus, the biomarkers (CSF, blood) will tell you, also the imaging biomarkers, that is PET biomarkers; but magnetic resonance tomography is not helpful because brain atrophy may come later, so only when you do have already dementia:there's a large variability regarding the prevalence of the brain to develop atrophy. Thus you may have a person with early Alzheimer’s dementia with completely normal MRI scan. Even some neuroradiologists don't know this, they think “oh the MRI scan is completely normal, it cannot be Alzheimer’s dementia”. This is completely wrong. 20% of the patients with early Alzheimer’s dementia have a completely normal MRI scan, but they will not have a completely normal CSF pattern of those molecular dementia biomarkers, they are much more reliable -or the Amyloid PET, where you can really image those plaques of aggregated peptides with isotope labeled compounds which are injected into the blood. They pass the blood brain barrier, and then you can imagine these toxic plaques – Aβ-plaques. Thus we have those biomarkers in cerebrospinal fluid, moreover(amyloid) positron emission tomography called Amyloid-PET, and now there's Tau-PET available. You can image tau protein, within the neurofibrillary tangles, that is aggregated tau. With Amyloid-PET you can image aggregated amyloid peptides. But PET s is really expensive, one scan costs more or less 2,000 euros. However, the blood assay may cost, only 60-70 euros. Thus it will be possible to do this (the diagnostics) by blood tests and this would be also really important for China because you can screen millions of people who are at risk and who may say “oh I think my memory has a problem and this the case all the day, all weeks, all months, but I am not depressed, so I think this is a problem”. Our blood tests already at this early preclinical stage clearly tell, if this is due to emerging Alzheimer's dementia or not. This gives a chance to develop the most efficient preventive strategies worldwide. Now the development of this blood biomarker guided preclinical diagnostics is also very important to speed up the development of novel preventive therapies because now you can do cost effective head-to-head clinical trials worldwide to identify the most efficient combination therapies to prevent Alzheimer’s dementia, to have a very efficient disease modification.
To summarize this, with standard clinical tools, with conventional neuropsychological tools you cannot really differentiate memory deficits in the elderly, that is if they are is due to emerging Alzheimer’s dementia on the background of Alzheimer's disease or depression or some something else. I did this as a young doctor for years in the memory clinics. Even a really experienced dementia expert can’t do this. You need biomarkers to do this.
8. You are a neo-classical music composer in addition to being a neuropsychiatrist. How do these two roles interact with one another?
Actually, these are two lives but I try to separate them as much as I can. But it becomes more and moreless, successful because it gets known and known I am asked more often by international colleagues if pieces of my music can be played when there's a prize lecture within a conference, to have a piano concert; and I have been asked now to compose a film music for the end credits of a new film. I started to compose when I was, maybe, fourteen or fifteen years old, but I did this for decades just on my own. But then my friends and patients said “oh, we like it very much you should produce a CD and put the pieces into notation ”. And then I entered a cooperation with real professional musicians like Shogher Hoveyan who last year won the Paris Piano Festival among two thousand pianists – winning the gold medal. She is a worldwide known pianist;andor Hayrapet Arakelyan who is a star in saxophone. Together with those really advanced musicians I produced the CD called EISREGEN (ICE RAIN).

9. What’s the most fascinating part of your profession as a medical doctor?
That is, in medicine, you have such a large variety of issues you can do, like from surgery, to psychotherapy and psychiatry. This is really fascinating, if you study medicine afterwards you have a large field where you can choose from, what you want to specialize in; and if you can be really successful in therapies, especially in psychiatry, which a lot of people don't know, that the effect size you have in psychiatry is much higher than in neurology, most people don't know this. You will not remove schizophrenia, or you will not remove depression, but the medical doctor does also not remove diabetes by putting new islet cells into the pancreas, he treats the insulin dysmetabolism by drugs but he doesn't remove diabetes. The psychiatrist can more and more efficiently treat, shorten and suppress the episode of depression or schizophrenia, but this with a high success rate. If you have experienced patients with a severe catatonic or stupor depression - where he would not be paralyzed -, there's fresh water in the room coming from the tap but he's depressed to such an extent that he will die from dehydration, even having fresh water next to him. Because if you suffer from really severe depression, you have such a significant stupor that you more or less can not do anything anymore. And if you then, for example, initiate treatment by electroconvulsive therapy or potent antidepressants, you can remove this condition within three to four weeks, and then the patient is as successful in cognition and everything as he or she has been before. It's really rewarding and most people don't know this.
10. What would you have been if you had not been a medical doctor?
To be honest, I don't know. I really don't know. I was asked by my teachers to study philosophy and languages because I had some talent in these areas, they thought. I really don't know.
I would not have become a musician and I wouldn't advise also my kids or anybody to do this as a career because it's so tough. Only one out of thousands can manage to make a really good living from this. Most professional musicians have to teach students and have low incomes. It is unpredictable and there’s such a high competition worldwide in piano or in violin, whatever. I wouldn't advise my kids to do this.
11. What are your hobbies during your leisure time?
Yes, of course composing -and I like to sail because I was raised at the north sea. I like the sea. When I was really young I did competitional rowing really on races, but only when I was really young. Now I do a little bit of jogging and different sports, but mostly doing music.
